Prevalence and Factors Associated with Antepartum Depression: A University Hospital-Based
DOI:
https://doi.org/10.33192/Smj.2021.84Keywords:
Antepartum, Associated factors, Depression, Pregnancy, PrevalenceAbstract
Objective: This study aimed to assess the prevalence of and factors associated with antepartum depression among Thai women.
Materials and Methods: All pregnant women attending the Antenatal Care Clinic at Songklanagarind Hospital from June to August 2020 were invited to participate and evaluated through self-administered questionnaires. Multivariate logistic regression models were used for the data analysis in order to control for potential confounders.
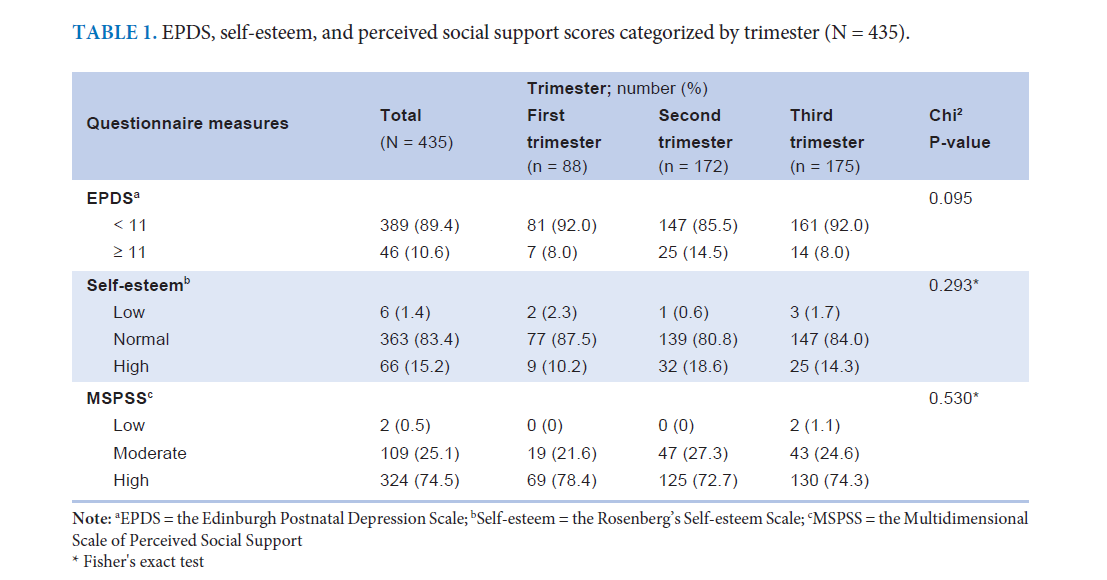
Results: 435 women were in their first, second, and third trimester of pregnancy (20.2 %, 39.5 %, and 40.2 %, respectively). The majority of them reported normal Rosenberg’s Self-esteem Scale scores (83.4 %) and a high level of perceived social support (74.5 %). Moreover, according to the Edinburgh Postnatal Depression Scale (EPDS) scores, the prevalence of antepartum depression was 10.6 %. A multivariate logistic regression analysis showed that factors associated with antepartum depression were second trimester of pregnancy, survival and below-survival levels of income, unintended pregnancy, and low level of self-esteem.
Conclusion: One-tenth of pregnant Thai women suffered from depression. Advanced gestational age, low income, unintended pregnancy, and low self-esteem were significant factors associated with antepartum depression.
References
2. Kittirattanapaiboon P, Tantirangsee N, Chutha W, Tanaree A, Kwansanit P, Assanangkornchai S, et al. Thai mental health survey working group 1bureau of mental health service administration, department of mental health. prevalence of mental disorders and mental health problems: results from Thai national mental health survey 2013. Bangkok: Bureau of Mental Health Service Administration, Department of Mental Health; 2016.
3. Sadock B, Sadock V, Ruiz P. Synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Philadelphia: Lippincott Williams & Wilkins, 2014.
4. Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet 2014;384:1775-88.
5. Burt V, Hendrick V. Clinical manual of women's mental health. Arlington (VA): American Psychiatric Publishing, 2005.
6. Grigoriadis S, VonderPorten E, Mamisashvili L, Tomlinson G, Dennis C, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes. J Clin Psychiatry 2013;74:e321-41.
7. Straub H, Adams M, Kim J, Silver R. Antenatal depressive symptoms increase the likelihood of preterm birth. Am J Obstet Gynecol 2012;207(4):329:e1-4.
8. Yonkers K, Wisner K, Stewart D, Oberlander T, Dell D, Stotland N, et al. The management of depression during pregnancy: a report from the American psychiatric association and the American college of obstetricians and gynecologists. Gen Hosp Psychiatry 2009;31(5):403-13.
9. Carter D, Kostaras X. Psychiatric disorders in pregnancy. BC Med J 2005;47:96-9.
10. Kids C. Depression in pregnant women and mothers: how it affects you and your child - caring for kids [Internet]. Ottawa: Canadian Paediatric Society. 2019 [cited 2019 Sept 8]. Available from: https://www.caringforkids.cps.ca/handouts/depression_in_ pregnant_women_ and_mothers.
11. Kaiyo-Utete M, Dambi JM, Chingono A, Mazhandu FSM, Madziro-Ruwizhu TB, Henderson C, et al. Antenatal depression: an examination of prevalence and its associated factors among pregnant women attending Harare polyclinics. BMC Pregnancy and Childbirth 2020;20:197.
12. Ogbo F, Eastwood J, Hendry A, Jalaludin B, Agho K, Barnett B, et al. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 2018;18:49.
13. Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systemic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Discord 2017;219:86-92.
14. Okagbue H, Adamu P, Bishop S, Oguntunde P, Opanuga A, Akhmetshin E. Systematic review of prevalence of antepartum depression during the trimesters of pregnancy. Maced J Med Sci 2019;7:1555-60.
15. Gebremichael G, Yihune M, Ajema D, Haftu D, Gedamu G. Perinatal depression and associated factors among mothers in southern Ethiopia: evidence from Arba Minch Zuria health and demographic surveillance site. Psychiatry J 2018;2018:7930684.
16. Bitew T, Hanlon C, Kebede E, Honikman S, Fekadu A. Antenatal depressive symptoms and perinatal complications: a prospective study in rural Ethiopia. BMC Psychiatry 2017;17:301.
17. Hu Y, Wang Y, Wen S, Guo X, Xu L, Chen B, et al. Association between social and family support and antenatal depression: a hospital-based study in Chengdu, China. BMC pregnancy and childbirth 2019;19:420.
18. Mohammad K, Gamble J, Creedy D. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 2011;27:e238-45.
19. Ongeri L, Otieno P, Mbui J, Juma E, Mathai M. Antepartum risk factors for postpartum depression: a follow up study among urban women living in Nairobi, Kenya. J Preg Child Health 2016;3:288.
20. Fransson E, Ortenstrand A, Hjelmstedt A. Antenatal depressive symptoms and preterm birth: a prospective study of a Swedish National sample. Birth 2010;38:10-6.
21. Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord 2008;108:147-57.
22. Babu GR, Murthy GVS, Singh N, Nath A, Rathnaiah M, Saldanha N, et al. Sociodemographic and medical risk factors associated with antepartum depression. Front Public Health 2018;6:127.
23. Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS One 2019;14:e0214992.
24. Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relation, and wealth in women in northern Tanzania: a cross-sectional study. BMC Women Health 2015;15:68.
25. Sitdhiraksa N, Nandidarbha R, Limsrichareon K, Thitadilok W. The prevalence of major depressive disorder during pregnancy at the antenatal care clinic Siriraj hospital. J Psychiatr Assoc Thailand 2010;55:15-26.
26. Wongpakaran T, Wongpakaran N. Confirmatory factor analysis of Rosenberg self-esteem scale: a study of Thai student sample. J Psychiatr Assoc Thailand 2011;56:59-70.
27. Rosenberg M. Society and the Adolescent Self-Image. New Jersey: Princeton University Press, 1965.
28. Wongpakaran T, Wongpakaran N, Ruktrakul R. Reliability and Validity of the Multidimensional Scale of Perceived Social Support (MSPSS): Thai Version. Clin Pract Epidemiol Ment Health 2011;7:161-6.
29. Zimet GD, Dahlem N, Zimet SG, Farley G. The multidimensional scale of perceived social support. J Pers Assess 1988;52:30-41.
30. Vacharaporn K, Pitanupong J, Samangsri N. Development of the Edinburgh Postnatal Depression Scale Thai version. J Ment Health Thai 2003;11:164-9.
31. Health M. What is The Best Screening Tool for Antenatal Depression. Boston: The MGH Center for Women's Mental Health [Internet]. 2015 [cited 2016 Sept 9]. Available from: https://womensmentalhealth.org/posts/what-is-the-best-screening-tool-for-antenatal-depression/.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














