Clinical Outcomes of Extracranial Germ Cell Tumors: A Single Institute’s Experience
DOI:
https://doi.org/10.33192/Smj.2021.87Keywords:
Extracranial Germ Cell Tumor, EGCT, Survival Rate, Treatment Outcome, ThailandAbstract
Objective: To determine the clinical features and treatment outcomes of pediatric extracranial germ cell tumor (EGCT) in Thailand.
Materials and methods: A retrospective chart review of children under 15 years old with newly diagnosed EGCT who were treated at Faculty of Medicine Siriraj Hospital from January, 2004 to December, 2013 was conducted.
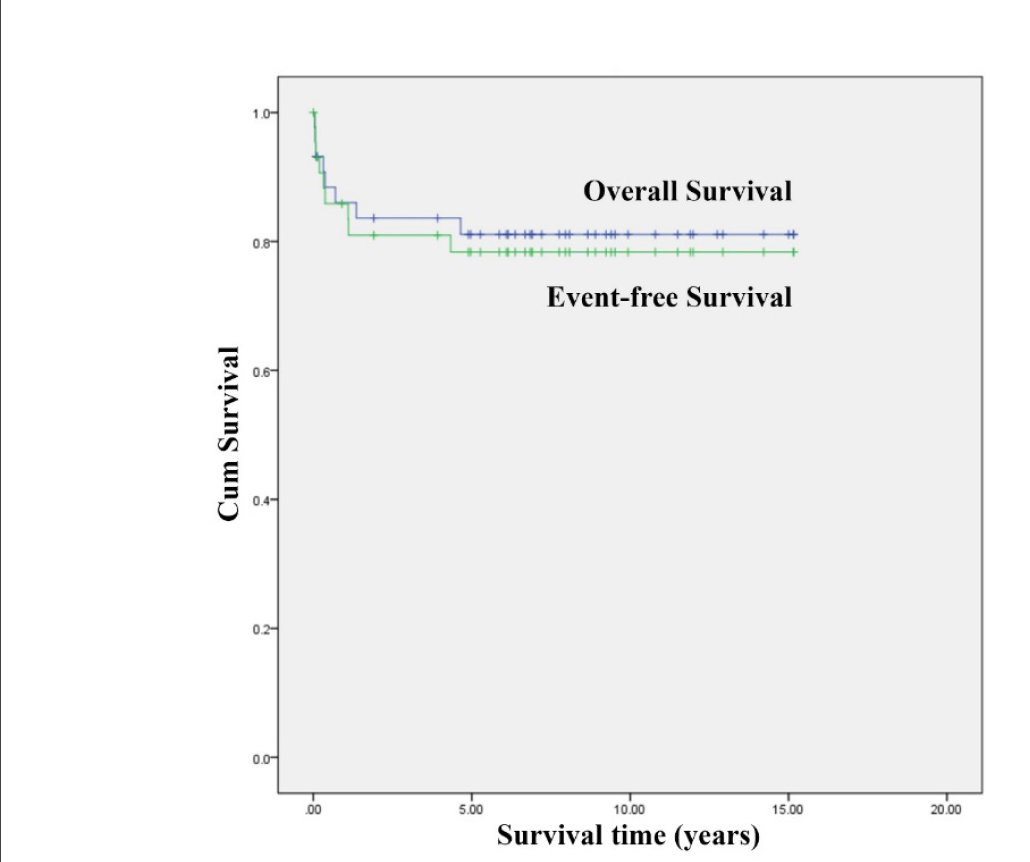
Results: Forty-four patients were included in the study. The median age at diagnosis was 1.74 years (1 day-14.7 years) with the median follow up time of 6.9 years (14 days-15.2 years). Twenty-eight patients (64%) had extragonadal tumor. The most common primary tumor location was the sacrococcygeal area. Majority of the patients (61%) had malignant EGCT; yolk sac tumor was the most common diagnosis. Six patients (14%) had stage IV disease. Forty patients (91%) underwent surgery; 27 patients (61%) received chemotherapy. Thirty-eight patients (86%) achieved remission; 3 patients (7%) subsequently relapsed at a median time of 1 year. Eight patients (18%) died, mostly from tumor progression. The 5-year event-free survival (EFS) and overall survival (OS) rate were 78.3% and 81.1%, respectively. Patients achieving total tumor removal had significantly better 5-year EFS and OS. Cox regression analysis revealed that the adequacy of surgery was the only prognostic factor for survival.
Conclusion: The survival rate of pediatric EGCT in our study was relatively favorable, but still inferior to that of developed countries. Novel therapy may be warranted for those patients who are unresponsive to the current treatment.
References
Kaatsch P, Hafner C, Calaminus G, Blettner M, Tulla M. Pediatric germ cell tumors from 1987 to 2011: Incidence rates, time trends, and survival. Pediatrics. 2015;135(1):e136-43.
Matsumoto F, Shimada K, Ida S. Tumors of bilateral streak gonads in patients with disorders of sex development containing y chromosome material. Clin Pediatr Endocrinol. 2014;23(3):93-7.
Piazza MJ, Urbanetz AA. Germ cell tumors in dysgenetic gonads. Clinics (Sao Paulo). 2019;74:e408.
Williams LA, Pankratz N, Lane J, Krailo M, Roesler M, Richardson M, et al. Klinefelter syndrome in males with germ cell tumors: A report from the children's oncology group. Cancer. 2018;124(19):3900-8.
De Backer A, Madern GC, Pieters R, Haentjens P, Hakvoort-Cammel FG, Oosterhuis JW, et al. Influence of tumor site and histology on long-term survival in 193 children with extracranial germ cell tumors. Eur J Pediatr Surg. 2008;18(1):1-6.
Wiangnon S, Veerakul G, Nuchprayoon I, Seksarn P, Hongeng S, Krutvecho T, et al. Childhood cancer incidence and survival 2003-2005, thailand: Study from the thai pediatric oncology group. Asian Pac J Cancer Prev. 2011;12(9):2215-20.
Olson TA, Murray MJ, Rodriguez-Galindo C, Nicholson JC, Billmire DF, Krailo MD, et al. Pediatric and adolescent extracranial germ cell tumors: The road to collaboration. J Clin Oncol. 2015;33(27):3018-28.
Rogers PC, Olson TA, Cullen JW, Billmire DF, Marina N, Rescorla F, et al. Treatment of children and adolescents with stage ii testicular and stages i and ii ovarian malignant germ cell tumors: A pediatric intergroup study--pediatric oncology group 9048 and children's cancer group 8891. J Clin Oncol. 2004;22(17):3563-9.
Sowithayasakul P, Sinlapamongkolkul P, Treetipsatit J, Vathana N, Narkbunnam N, Sanpakit K, et al. Hematologic malignancies associated with mediastinal germ cell tumors: 10 years' experience at thailand's national pediatric tertiary referral center. J Pediatr Hematol Oncol. 2018;40(6):450-5.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: Revised recist guideline (version 1.1). Eur J Cancer. 2009;45(2):228-47.
Schneider DT, Calaminus G, Koch S, Teske C, Schmidt P, Haas RJ, et al. Epidemiologic analysis of 1,442 children and adolescents registered in the german germ cell tumor protocols. Pediatr Blood Cancer. 2004;42(2):169-75.
Hasle H. Pattern of malignant disorders in individuals with down's syndrome. Lancet Oncol. 2001;2(7):429-36.
Liu J, Krantz ID. Cornelia de lange syndrome, cohesin, and beyond. Clin Genet. 2009;76(4):303-14.
Maruiwa M, Nakamura Y, Motomura K, Murakami T, Kojiro M, Kato M, et al. Cornelia de lange syndrome associated with wilms' tumour and infantile haemangioendothelioma of the liver: Report of two autopsy cases. Virchows Arch A Pathol Anat Histopathol. 1988;413(5):463-8.
Nichols CR, Roth BJ, Heerema N, Griep J, Tricot G. Hematologic neoplasia associated with primary mediastinal germ-cell tumors. N Engl J Med. 1990;322(20):1425-9.
Bosl GJ, Ilson DH, Rodriguez E, Motzer RJ, Reuter VE, Chaganti RS. Clinical relevance of the i(12p) marker chromosome in germ cell tumors. J Natl Cancer Inst. 1994;86(5):349-55.
Faure-Conter C, Pashankar F. Immature ovarian teratoma: When to give adjuvant therapy? J Pediatr Hematol Oncol. 2017;39(7):487-9.
Mann JR, Gray ES, Thornton C, Raafat F, Robinson K, Collins GS, et al. Mature and immature extracranial teratomas in children: The uk children's cancer study group experience. J Clin Oncol. 2008;26(21):3590-7.
Marina NM, Cushing B, Giller R, Cohen L, Lauer SJ, Ablin A, et al. Complete surgical excision is effective treatment for children with immature teratomas with or without malignant elements: A pediatric oncology group/children's cancer group intergroup study. J Clin Oncol. 1999;17(7):2137-43.
Rescorla FJ, Sawin RS, Coran AG, Dillon PW, Azizkhan RG. Long-term outcome for infants and children with sacrococcygeal teratoma: A report from the childrens cancer group. J Pediatr Surg. 1998;33(2):171-6.
Cushing B, Giller R, Cullen JW, Marina NM, Lauer SJ, Olson TA, et al. Randomized comparison of combination chemotherapy with etoposide, bleomycin, and either high-dose or standard-dose cisplatin in children and adolescents with high-risk malignant germ cell tumors: A pediatric intergroup study--pediatric oncology group 9049 and children's cancer group 8882. J Clin Oncol. 2004;22(13):2691-700.
Necchi A, Mariani L, Di Nicola M, Lo Vullo S, Nicolai N, Giannatempo P, et al. High-dose sequential chemotherapy (hds) versus peb chemotherapy as first-line treatment of patients with poor prognosis germ-cell tumors: Mature results of an italian randomized phase ii study. Ann Oncol. 2015;26(1):167-72.
Frazier AL, Hale JP, Rodriguez-Galindo C, Dang H, Olson T, Murray MJ, et al. Revised risk classification for pediatric extracranial germ cell tumors based on 25 years of clinical trial data from the United Kingdom and United States. J Clin Oncol. 2015;33(2):195-201.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














