Speech Outcome Analysis after Primary Cleft Palate Repair: Interim Siriraj Hospital Audit
DOI:
https://doi.org/10.33192/Smj.2021.96Keywords:
Cleft palate, speech outcome, velopharyngeal insufficiency, craniofacial abnormalitiesAbstract
Objective: To evaluate the speech outcomes after primary cleft palate repair in a single tertiary medical institution of Thailand.
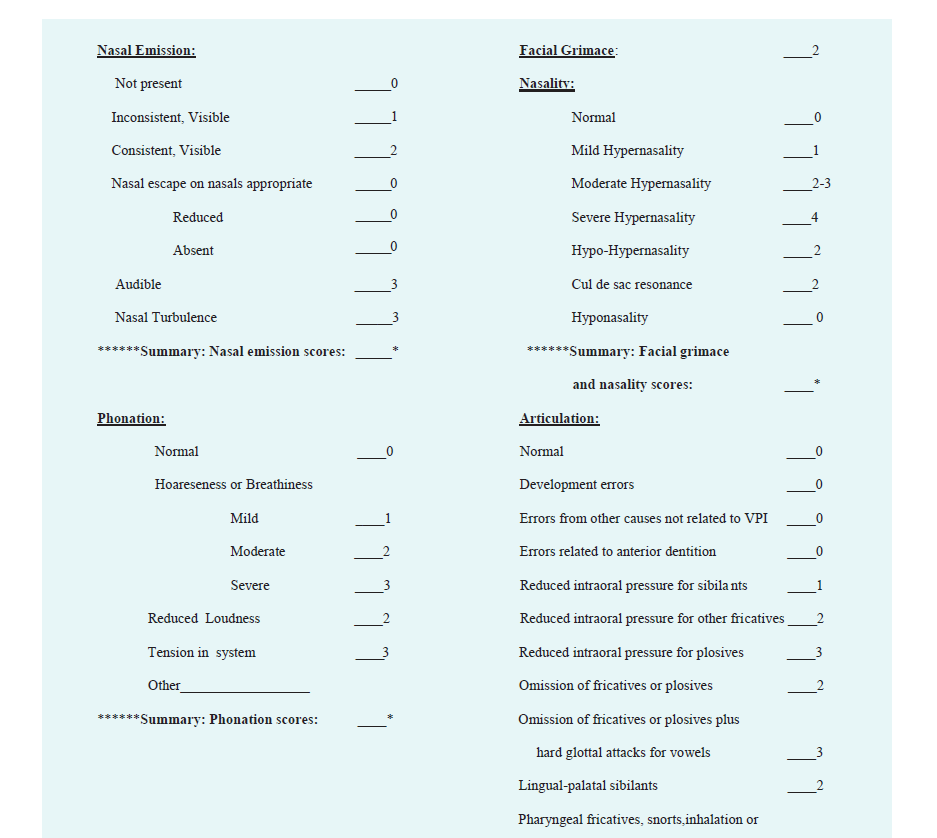
Materials and Methods: A prospective cohort study was performed. Patients who had cleft palate with/without cleft lip and underwent primary cleft palate repair were included. Speech assessment was performed using the Pittsburgh weighted speech score (PWSS) by a speech-language pathologist.
Results: Forty patients (21 males and 19 females) who underwent primary cleft palate repair at Siriraj Hospital were included. The median age at the time of speech evaluation was 7 years. The median age at primary cleft palate surgery was 12 months. The predominant cleft palate type was Veau 3 (47.5%). Oronasal fistula occurred 40%. Two-flap palatoplasty and intravelar veloplasty were the most common procedures. Median PWSS was 7, in which the competence velopharyngeal mechanism was found 5%, borderline competence 10%, borderline incompetence 32.5%, and incompetence velopharyngeal mechanism 52.5%. Among the velopharyngeal incompetence group, articulation disorder was the most common disorder with median score of 3. Besides, the median scores for hypo/hyper-nasality, nasal emission, phonation, and facial grimace disorder were 1, 2, 0 and 0, respectively. There was no statistically significant association between velopharyngeal incompetence and cleft types, age at primary surgery, type of operation, the width of cleft palate and prevalence of postoperative oronasal fistula or otitis media effusion.
Conclusion: Velopharyngeal incompetence has been commonly identified after cleft palate repair in our institute. The articulation disorder is the most common characteristic.
References
2. Chowchuen B, Surakunprapha P, Winaikosol K, Punyavong P, Kiatchoosakun P, Pradubwong S. Birth Prevalence and Risk Factors Associated With CL/P in Thailand. Cleft Palate Craniofac J 2021;58(5):557-66.
3. Fisher DM, Sommerlad BC. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg 2011;128(4):342e-60e.
4. Gart MS, Gosain AK. Surgical management of velopharyngeal insufficiency. Clin Plast Surg 2014;41(2):253-70.
5. Bicknell S, McFadden LR, Curran JB. Frequency of pharyngoplasty after primary repair of cleft palate. J Can Dent Assoc 2002;68(11):688-92.
6. Bickner R, Hudak T. THE NATURE OF "STANDARD" THAI. Journal of South Asian Literature 1990;25(1):163-75.
7. Prathanee B, Lorwatanapongsa P, Makarabhirom K, Wattanawongsawang W. Thai speech and language norms for children 2 1/2 to 4 years of age. J Med Assoc Thai 2010;93 (Suppl 4):S7-15.
8. Henningsson G, Kuehn DP, Sell D, Sweeney T, Trost-Cardamone JE, Whitehill TL. Universal parameters for reporting speech outcomes in individuals with cleft palate. Cleft Palate Craniofac J 2008;45(1):1-17.
9. Kummer AW, Clark SL, Redle EE, Thomsen LL, Billmire DA. Current practice in assessing and reporting speech outcomes of cleft palate and velopharyngeal surgery: a survey of cleft palate/craniofacial professionals. Cleft Palate Craniofac J 2012 ;49(2):146-52.
10. McWilliams BJ, Phillips BJ. Velopharyngeal Incompetence: Audio Seminars in Speech Pathology. Philadelphia: W. B. Saunders, Inc, 1979.
11. Veau V. Division Palatine: Anatomie, Chirurgie, Phone´tique. Paris: Masson, 1931.
12. Persson C, Elander A, Lohmander-Agerskov A, Söderpalm E. Speech outcomes in isolated cleft palate: impact of cleft extent and additional malformations. Cleft Palate Craniofac J 2002;39:397-408.
13. Nyberg J, Westberg LR, Neovius E, Larson O, Henningsson G. Speech results after one-stage palatoplasty with or without muscle reconstruction for isolated cleft palate. Cleft Palate Craniofac J 2010;47:92-103.
14. Klintö K, Salameh EK, Svensson H, Lohmander A. The impact of speech material on speech judgement in children with and without cleft palate. Int J Lang Commun Disord 2011;46(3):348-60.
15. Britton L, Albery L, Bowden M, Harding-Bell A, Phippen G, Sell D. A cross-sectional cohort study of speech in five-year-olds with cleft palate ± lip to support development of national audit standards: benchmarking speech standards in the United Kingdom. Cleft Palate Craniofac J. 2014;51(4):431-51.
16. Dissaux C, Grollemund B, Bodin F, Picard A, Vazquez MP, Morand B, et al. Evaluation of 5-year-old children with complete cleft lip and palate: Multicenter study. Part 2: Functional results. J Craniomaxillofac Surg 2016;44(2):94-103.
17. Prathanee B, Pumnum T, Seepuaham C, Jaiyong P. Five-year speech and language outcomes in children with cleft lip-palate. J Craniomaxillofac Surg 2016;44(10):1553-60.
18. Ooppanasak N, Makarabhirom K, Chowchuen B, Prathanee B. Speech Outcomes in Children with Cleft and Palate: Srinagarind Hospital, Khon Kaen University, Thailand. J Med Assoc Thai 2019;102:10.
19. Albustanji YM, Albustanji MM, Hegazi MM, Amayreh MM. Prevalence and types of articulation errors in Saudi Arabic-speaking children with repaired cleft lip and palate. Int J Pediatr Otorhinolaryngol 2014;78(10):1707-15.
20. Ha S, Koh KS, Moon H, Jung S, Oh TS. Clinical Outcomes of Primary Palatal Surgery in Children with Nonsyndromic Cleft Palate with and without Lip. Biomed Res Int 2015;2015:185459.
21. Abou-Elsaad T, Baz H, Afsah O, Mansy A. The nature of articulation errors in Egyptian Arabic-speaking children with velopharyngeal insufficiency due to cleft palate. Int J Pediatr Otorhinolaryngol 2015;79(9):1527-32.
22. Dorf DS, Curtin JW. Early cleft palate repair and speech outcome. Plast Reconstr Surg 1982;70(1):74-81.
23. Prathanee B, Dechongkit S, Manochiopinig S. Development of community-based speech therapy model: for children with cleft lip/palate in northeast Thailand. J Med Assoc Thai 2006;89(4):500-8.
24. Setabutr D, Sathavornmanee T, Jitpakdee P, Nudchawong S, Krergmatukorn P. The Trend of Cleft Care at a Children's Referral Center in Thailand. Cleft Palate Craniofac J 2020;57(9):1100-4.
25. Kaewkumsan N, Chowchuen B, Prathanee B. Clinical outcomes of primary palatoplasty in preschool-aged cleft palate children in Srinagarind Hospital and comparison with other standard cleft centers. J Med Assoc Thai 2014;97(Suppl 10):S37-48.
26. Jackson MS, Jackson IT, Christie FB. Improvement in speech following closure of anterior palatal fistulas with bone grafts. Br J Plast Surg 1976;29(4):295-96.
27. Abyholm FE, Borchgrevink HH, Eskeland G. Palatal fistulae following cleft palate surgery. Scand J Plast Reconstr Surg 1979;13(2):295-300.
28. Murthy AS, Parikh PM, Cristion C, Thomassen M, Venturi M, Boyajian MJ. Fistula after 2-flap palatoplasty: a 20-year review. Ann Plast Surg 2009;63(6):632-5.
29. Stewart TL, Fisher DM, Olson JL. Modified Von Langenbeck cleft palate repair using an anterior triangular flap: decreased incidence of anterior oronasal fistulas. Cleft Palate Craniofac J 2009;46(3):299-304.
30. Eberlinc A, Koželj V. Incidence of residual oronasal fistulas: a 20-year experience. Cleft Palate Craniofac J 2012;49(6):643-8.
31. Hortis-Dzierzbicka M, Radkowska E, Fudalej PS. Speech outcomes in 10-year-old children with complete unilateral cleft lip and palate after one-stage lip and palate repair in the first year of life. J Plast Reconstr Aesthet Surg 2012;65(2):175-81.
32. Saothonglang K, Punyavong P, Winaikosol K, Jenwitheesuk K, Surakunprapha P. Risk Factors of Fistula Following Primary Palatoplasty. J Craniofac Surg 2021;32(2):587-90.
33. Ungkanont K, Boonyabut P, Komoltri C, Tanphaichitr A, Vathanophas V. Surveillance of Otitis Media with Effusion in Thai Children With Cleft Palate: Cumulative Incidence and Outcome of the Management. Cleft Palate Craniofac J 2018;55(4):590-5.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














