Sacral Neuromodulation in the Treatment of Non-Neurogenic Female Lower Urinary Tract Dysfunction; First Case-series and Systematic Review of Literature
DOI:
https://doi.org/10.33192/Smj.2021.94Keywords:
Lower urinary tract dysfunction, female, sacral neuromodulationAbstract
Objective: To demonstrate which types of non-neurogenic female lower urinary tract dysfunction (LUTD) respond to sacral neuromodulation (SNM) after the failure of all non-invasive treatments.
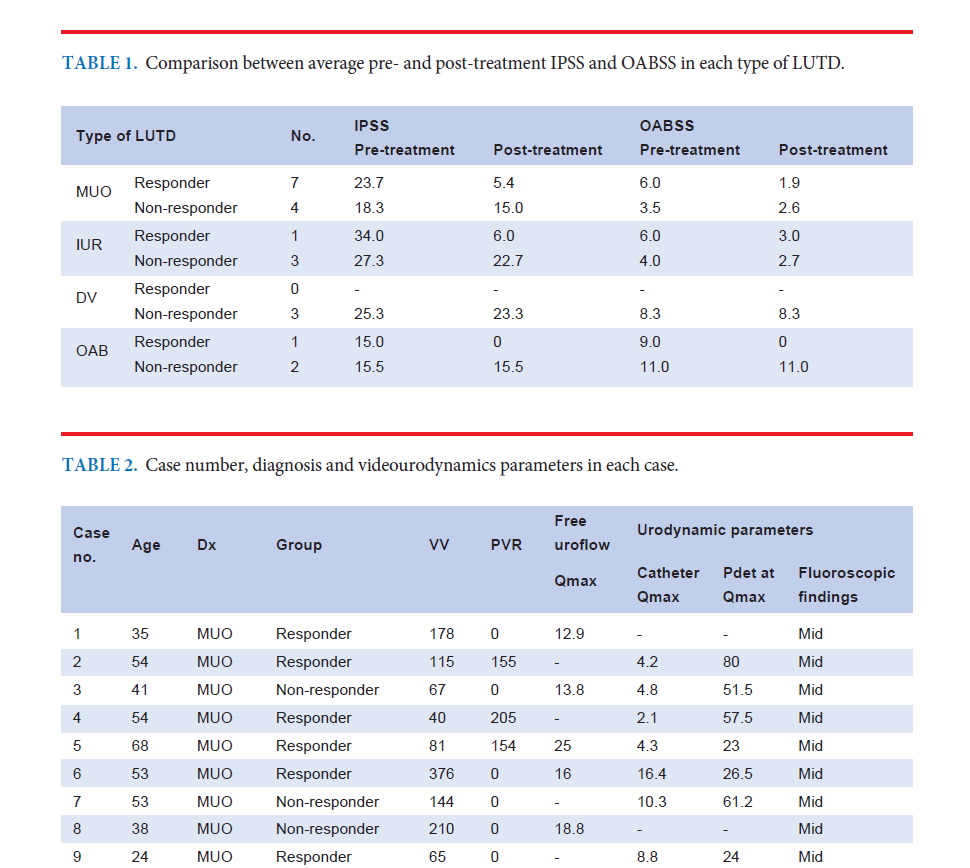
Materials and Methods: Female LUTD performed SNM between 2017 and 2019 were retrospectively reviewed. A case with anatomical or neurological abnormalities were excluded by thorough physical examination and investigations. The specific type of LUTD, including midurethral obstruction (MUO), was diagnosed by videourodynamics (VUDS). Clinical diagnoses, including idiopathic urinary retention (IUR), voiding dysfunction (VD) and refractory overactive bladder (OAB), were used instead of VUDS diagnosis when the result was normal or inconclusive. The International Prostate Symptom Score (IPSS) and Overactive Bladder Symptom Score (OABSS) in Thai version were used to compare between pre and post-treatment. Responder was defined as an IPSS and/or OABSS decreased more than 50% from baseline.
Results: Total 21 cases were performed SNM. The average age was 49.6 (24–80) years. The average pre-treatment IPSS and OABSS were 23.4 and 6.4 as well as average post-treatment IPSS and OABSS were 13.7 and 3.8. Only 9 out of 21 cases (42.9%) showed improvement after SNM. The responders included 7 out of 11 MUO (63.6%), 1 out of 4 IUR (25.0%), and 1 out of 3 OAB (33.3%). None of the VD cases responded to SNM.
Conclusion: SNM is another option for female patients with LUTD who have failed to respond to conservative treatments. After completely excluding anatomical and neurological abnormalities, the types of LUTD having a chance to respond to SNM are MUO, IUR, and OAB.
References
2. Liberman D, Ehlert MJ, Siegel SW. Sacral Neuromodulation in Urological Practice. Urology. 2017;99:14-22.
3. Rosier P, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, et al. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017;36(5):1243-60.
4. Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-20.
5. Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn. 2000;19(5):553-64.
6. Nontakaew K, Kochakarn W, Kijvika K, Viseshsindh W, Silpakit C. Reliability of a Thai version of the International Prostate Symptom Score (IPSS) for the Thai population. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2014;97(6):615-20.
7. Bunyavejchevin S. Reliability of Thai-Version Overactive Bladder Symptom Scores (OABSS) Questionnaire and the Correlations of OABSS with Voiding Diary, International Prostate Symptom Score (IPSS), and Patient Perception of Bladder Condition (PPBC) Questionnaires. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2015;98(11):1064-74.
8. Datta SN, Chaliha C, Singh A, Gonzales G, Mishra VC, Kavia RB, et al. Sacral neurostimulation for urinary retention: 10-year experience from one UK centre. BJU Int. 2008;101(2):192-6.
9. Rademakers KL, Drossaerts JM, van Kerrebroeck PE, Oelke M, van Koeveringe GA. Prediction of sacral neuromodulation treatment success in men with impaired bladder emptying-time for a new diagnostic approach. Neurourol Urodyn. 2017;36(3):808-10.
10. Chan G, Qu LG, Gani J. Evaluation of pre-operative bladder contractility as a predictor of improved response rate to a staged trial of sacral neuromodulation in patients with detrusor underactivity. World J Urol. 2020.
11. Noblett K, Siegel S, Mangel J, Griebling TL, Sutherland SE, Bird ET, et al. Results of a prospective, multicenter study evaluating quality of life, safety, and efficacy of sacral neuromodulation at twelve months in subjects with symptoms of overactive bladder. Neurourol Urodyn. 2016;35(2):246-51.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














