Psychometric Properties of the PHQ-9, HADS, and CES-D Questionnaires and the Prevalence of Depression in Patients with Cancer Receiving Radiotherapy
DOI:
https://doi.org/10.33192/Smj.2021.103Keywords:
PHQ-9, HADS, CES-D, Depression, Cancer, RadiotherapyAbstract
Objective: The primary aim was to compare the psychometric properties among the Patient Health Questionnaire (PHQ-9) (both including and excluding somatic symptom items), the depression subscale of the Hospital Anxiety and Depression Scale (HADS-D), and the Center for Epidemiologic Studies Depression Scale (CES-D) in detecting depression in cancer patients receiving radiotherapy. The secondary aim was to investigate the prevalence of depression in this group of patients.
Materials and Methods: Overall, 198 participants with cancer diagnosis from a radiology clinic took part in the study. They completed PHQ-9, HADS-D, and CES-D questionnaires and were interviewed in line with the Mini-International Neuropsychiatric Interview (M.I.N.I.) to confirm the diagnosis. The PHQ-9 was analyzed for three scoring methods: sum-score, inclusive (including all items), and exclusive (excluding 4 somatic symptom items) methods. The psychometric properties of each questionnaire were analyzed. The prevalence of depression measured by the M.I.N.I. was evaluated.
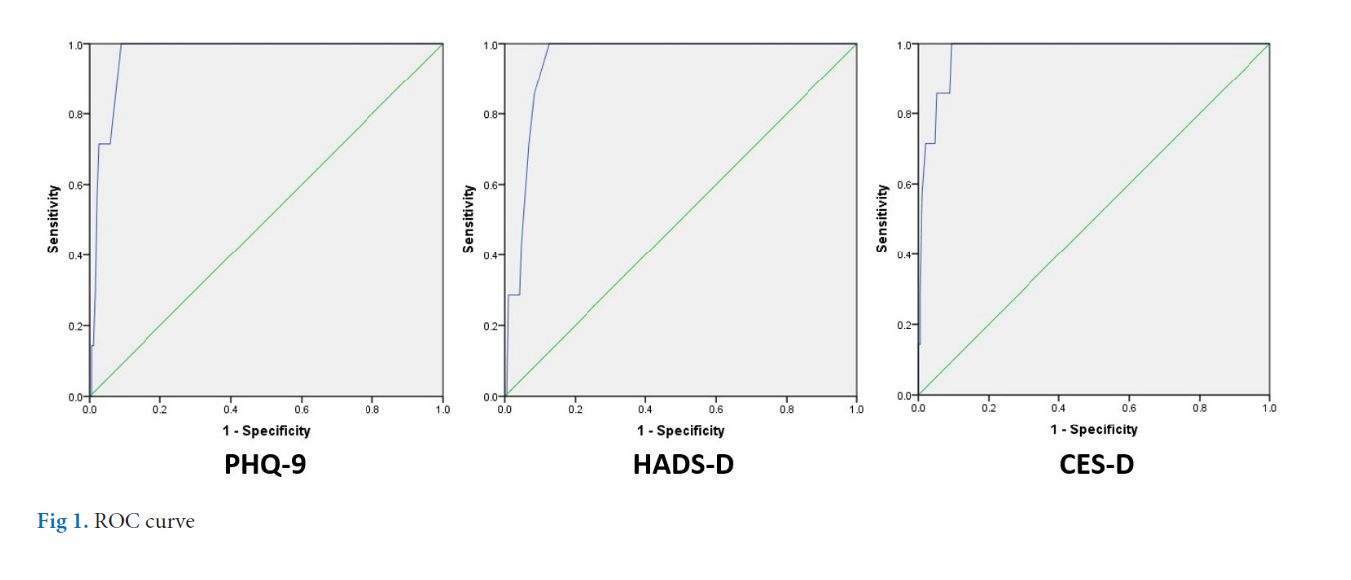
Results: The sum-score method of the PHQ-9 had an equal sensitivity (100%) to the HADS-D and CES-D, and had a slightly higher specificity (91.1%) than the HADS-D (87.4%) and CES-D (90.6%). When compared results within the PHQ-9, the sum-score method had greater sensitivity than the inclusive (71.4%) and exclusive (42.9%) methods, and had a slightly lower specificity than the inclusive (96.9%) and exclusive (97.4%) methods. The prevalence of depression assessed by the M.I.N.I was 3.5%.
Conclusion: The sum-score method of the PHQ-9 seemed to be the best tool to use for depression screening in cancer patients receiving radiotherapy due to its excellent sensitivity and specificity.
References
2. Pinquart M, Duberstein PR. Depression and cancer mortality: a metaanalysis. Psychological Medicine 2010;40:1797-810.
3. Smith HR. Depression in cancer patients: Pathogenesis, implications and treatment (Review). Oncology Letter 2015;9:1509-14.
4. Chochinov HM, Tataryn D, Clinch JJ, Dudgeon D. Will to live in the terminally ill. Lancet 1999;354:816-9.
5. Breirbart W, Rosenfeld B, Pessin H, Kaim M, Funesti-Esch J, Galietta M, Nelson CJ, Brescia R. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA 2000;284(22):2907-11.
6. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999;282(18):1737-44.
7. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70.
8. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1:385-401.
9. Vodermaier A, Linden W, Siu C. Screening for emotional distress in cancer patients: a systematic review of assessment instruments. J Natl Cancer Inst. 2009;101(21):1464-88.
10. Chhabria KS, Carnaby GD. Psychometric validation of the Center for Epidemiological Studies Depression Scale in Head and Neck Cancer patients. Oral Oncology 2017; 75:158-62.
11. Zimmerman M, Galione JN, Chelminski I, McGlinchey JB, Young D, Dalrymple K, Ruggero CJ, Witt CF. A simpler definition of major depressive disorder. Psychological Medicine 2010;40:451-7.
12. Lie HC, Hjermstad MJ, Fayers P, Finset A, Kaasa S, Loge JH. Depression in advanced cancer – Assessment challenges and associations with disease load. Journal of Affective Disorders 2015;173:176-84.
13. Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry 2008;8:46.
14. American Psychiatric Association. Diagnostic and statistical manual of mental disorder. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
15. Zimmerman M, Emmert-Aronson BO, Brown TA. Concordance between a simpler definition of major depressive disorder and diagnostic and statistical manual of mental disorders, fourth edition: an independent replication in an outpatient sample. Comprehensive Psychiatry 2011;52:261-4.
16. Nilchaikovit T, Lortrakul M, Phisansuthideth U. Development of Thai version of Hospital Anxiety and Depression Scale in cancer patients. J Psychiatr Assoc Thailand 1996;41(1):18-30.
17. Kuptniratsaikul V, Pekuman P. The study of the Center for Epidemiologic Studies-Depression Scale (CES-D) in Thai people. Siriraj Hosp Gaz 1997;49:442-8.
18. Kittirattanapaiboon P, Khamwongpin M. The Validity of the Mini International Neuropsychiatric Interview (M.I.N.I.)-Thai Version. Journal of Mental Health of Thailand 2005;13(3)c.
19. Streiner DL, Cairney J. What’s under the ROC? An introduction to receiver operating characteristics curves. Can J Psychiatry 2007;52(2):121-8.
20. George D, Mallery P. SPSS for Windows step by step: A simple guide and reference. 11.0 update (4th ed.). Boston: Allyn & Bacon; 2003.
21. Mitchell AJ, Lord K, Symonds P. Which symptoms are indicative of DSMIV depression in cancer settings? An analysis of the diagnostic significance of somatic and non-somatic symptoms. J Affect Disord 2012;138(1-2):137-48.
22. Hardman A, Maguire P, Crowther D. The recognition of psychiatric morbidity on a medical oncology ward. J Psychosom Res 1989;33:235-39.
23. Derogatis LR, Morrow GR, Fetting J, Penman D, Piasetsky S, Schmale AM, Henrichs M, Carnicke CL Jr. The prevalence of psychiatric disorders among cancer patients. JAMA 1983;249:751-57.
24. Kugaya A, Akechi T, Okuyama T, Okamura H, Uchitomi Y. Screening for psychological distress in Japanese cancer patients, Jpn J Clin Oncol 1998;28:333-38.
25. Lansky SB, List MA, Herrmann CA, Ets-Hokin EG, DasGupta TK, Wilbanks GD, Hendrickson FR. Absence of major depressive disorder in female cancer patients. J Clin Oncol 1985;3:1553-60.
26. Akechi T, Okuyama T, Sugawara Y, Nakano T, Shima Y, Uchitomi Y. Major depression, adjustments, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factors. J Clin Oncol 2004;22:1957-65.
27. Gandubert C, Carrière I, Escot C, Soulier M, Hermès A, Boulet 814 Volume 73, No.12: 2021 Siriraj Medical Journal https://he02.tci-thaijo.org/index.php/sirirajmedj/index P, Ritchie K, Chaudieu I. Onset and relapse of psychiatric disorders following early breast cancer: a case–control study. Psychooncology 2009;18:1029-37.
28. Razavi D, Delvaux N, Farvacques C, Robaye E. Screening for adjustment disorders and major depressive disorders in cancer in-patients. Br J Psychiatry 1990;156:79-83.
29. Park EM, Rosenstein DL. Depression in adolescents and young adults with cancer. Dialogues Clin Neurosci 2015;17(2):171-80.
30. Leeflang MM, Rutjes AW, Reitsma JB, Hooft L, Bossuyt PM. Variation of a test’s sensitivity and specificity with disease prevalence. CMAJ 2013;185(11):E537-E544.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














