The Relationship between Mental Health with the Level of Empathy Among Medical Students in Southern Thailand: A University-Based Cross- Sectional Study
DOI:
https://doi.org/10.33192/Smj.2021.108Keywords:
Empathy, mental health, medical studentAbstract
Objective: To determine the level of and factors associated with empathy among medical students.
Materials and Methods: This cross-sectional study surveyed all first- to sixth-year medical students at the Faculty
of Medicines, Prince of Songkla University, at the end of the 2020 academic year. The questionnaires consisted of:
1) The personal and demographic information questionnaire, 2) The Toronto Empathy Questionnaire, and 3) Thai
Mental Health Indicator-15. Data were analyzed using descriptive statistics, and factors associated with empathy
level were assessed via chi-square and logistic regression analyses.
Results: There were 1010 participants with response rate of 94%. Most of them were female (59%). More than half
(54.9%) reported a high level of empathy. There was a statistically significant difference in empathy levels between
pre-clinical and clinical medical students; in regards to empathy subgroups (P-value < 0.001). The assessment of
emotional states in others by demonstrating appropriate sensitivity behavior, altruism, and empathic responding
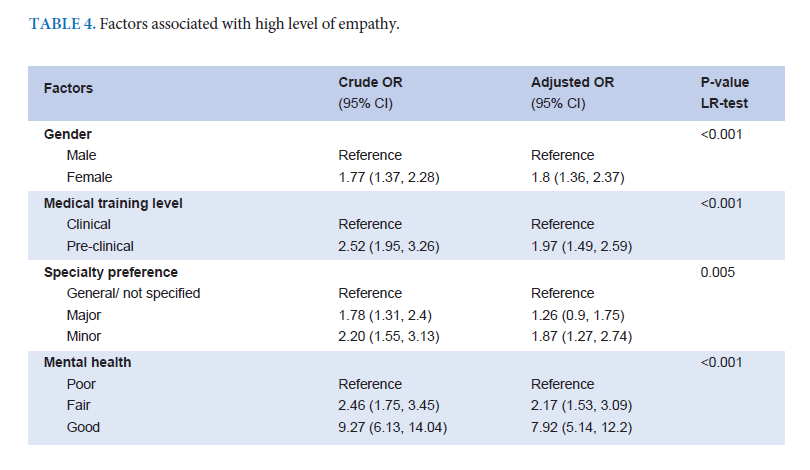
scores among the pre-clinical group were higher than those of the clinical group. Multivariate analysis indicated
that female gender, pre-clinical training level, and minor specialty preference were factors associated with empathy
level. The protective factor that significantly improved the level of empathy was having fair to good mental health.
Conclusion: More than half of the surveyed medical students reported a high level of empathy. The protective factor
that improved the level of empathy was good mental health. However, future qualitative methods, longitudinal
surveillance, or long-term follow-up designs are required to ensure the trustworthiness of these findings.
References
Pers 1972;40:525-43.
2. Cohen D, Strayer J.Empathy in conduct-disordered and
comparison youth. Dev Psychol 1996;32.988-98
3. Davis MH. Measuring individual differences in empathy: evidence
for a multidimensional approach. J Pers Soc Psychol 1983;44.
840 Volume 73, No.12: 2021 Siriraj Medical Journal https://he02.tci-thaijo.org/index.php/sirirajmedj/index
113-26.
4. Marcus ER. Empathy, humanism, and the professionalization
process of medical education. Acad Med 1999;74.1211-5.
5. Carre A, Stefaniak N, D’Ambrosio F, Bensalah L, Besche-
Richard C. The Basic Empathy Scale in Adults (BES-A): factor
Structure of a Revised Form. Psychol Assess 2013;25.679-91.
6. Buie DH. Empathy: its nature and limitations. J Am Psychoanal
Assoc 1981;29:281-307.
7. Elam CL. Use of “emotional intelligence” as one measure of
medical school applicants’ noncognitive characteristics. Acad
Med 2000;75:445-6.
8. Elam C, Stratton TD, Andrykowski MA. Measuring the emotional
intelligence of medical school matriculants. Acad Med 2001;76:
507-8.
9. Hirsch EM. The role of empathy in medicine: a medical student’s
perspective. AMA J Ethics 2007;9:423-7.
10. Larson EB, Yao X. Clinical empathy as emotional labor in the
patient physician relationship. JAMA 2005;293:1100-6.
11. Zinn W. The empathic physician. Arch Intern Med 1993;153:
306-12.
12. Halpern J. What is clinical empathy? J Gen Intern Med 2003;
18:670-4.
13. Adler HM. The history of the present illness as treatment:
who’s listening, and why does it matter? J Am Board Fam
Pract 1997;10:28-35.
14. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of
empathic communication in the medical interview. JAMA
1997;277:678-82.
15. Bellet PS, Maloney MJ. The importance of empathy as an
interviewing skill. JAMA 1991;266:1831-2.
16. Anfossi M, Numico G. Empathy in the doctor-patient relationship.
J Clin Oncol 2004;22:2258-9.
17. Chen D, Lew R, Hershman W, Orlander J. A Cross-sectional
Measurement of Medical Student Empathy. J Gen Intern Med
2007;22:1434-8.
18. Vitayanont A, Pitanupong J. Processes of communication.
Songkla Med J 2011;29:195-201.
19. Pitanupong J, Vitayanon A. Knowledge, attitude and insight
regarding communication skills in medical students. Songkla
Med J 2011;29:109-16.
20. Norphun N, Pitanupong J, Jiraphan A. Stress and Coping
Strategies among Thai Medical Students in a Southern Medical
School. Siriraj Med J 2020;72.238-244.
21. Jatchavala C, Pitanupong J. Resilience in Medical Doctors
within the Areas of the Southern Thailand Insurgency. Siriraj
Med J 2019;71.228-233.
22. Jumroonrojana K, Zartrungpak S. Development of the Jefferson
Scale of Physician Empathy-Student Version (Thai Version).
J Psychiatr Assoc Thailand 2012;57:213-24.
23. Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto
Empathy Questionnaire: scale development and initial validation
of a factor-analytic solution to multiple empathy measures. J
Pers Assess 2009;91:62-71.
24. Mongkol A, Huttapanom W. Thai Happiness Indicators (THI-
15) [monograph on the Internet]. Nonthaburi: Department
of Mental Health, Ministry of Public Health; 2011 [cited 2020
Oct 5] Available from: http://www.dmh.go.th/test/qtest/
25. Melanie N, Friedrich E, Diethard T, Martin RF, Markus W,
Christiane W, et al. Empathy decline and its reasons: a systematic
review of studies with medical students and residents. Acad
Med 2011;86:996-1009.
26. Hojat M, Shannon SC, DeSantis J, Speicher MR, Bragan L,
Calabrese LH. Does empathy decline in the clinical phase of
medical education? a nationwide, multi-institutional, crosssectional
study of students at do-granting medical schools.
Acad Med 2020;95:911-8.
27. Hojat M, Gonnella JS, Veloski J. Rebuttals to critics of studies
of the decline of empathy. Acad Med 2010;85:1812.
28. Newton BW. Rebuttals to critics of studies of the decline of
empathy. Acad Med 2010;85:1812-3.
29. Sherman JJ, Cramer AP. Rebuttals to critics of studies of the
decline of empathy. Acad Med 2010;85:1813.
30. Hemmerdinger JM, Stoddart SD, Lilford RJ. A systematic
review of tests of empathy in medicine. BMC Med Educ 2007;
7:24.
31. Pedersen R. Empirical research on empathy in medicine-A
critical review. Patient Educ Couns 2009;76:307-22.
32. Hojat M, Gonnella JS, Mangione S, Nasca TJ, Magee M.
Physician empathy in medical education and practice: experience
with the Jefferson Scale of physician empathy. Semin Integr
Med 2003;1:25-41.
33. Beckman HB, Frankel RM. Training practitioners to communicate
effectively in cancer care: it is the relationship that counts.
Patient Educ Couns 2003;50:85-9.
34. Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching
empathy to medical students: an updated, systematic review.
Acad Med 2013;88:1171-7.
35. Argent J, Faulkner A, Jones A, O’Keeffe C. Communication
skills in palliative care: development and modification of a
rating scale. Med Educ 1994;28,559-65.
36. Rosenthal S, Howard B, Schlussel YR, Herrigel D, Smolarz BG,
Gable B, et al. Humanism at heart: preserving empathy in
third-year medical students. Acad Med 2011;86:350-8.
37. Lim BT, Moriarty H, Huthwaite M. “Being-in-role”: a teaching
innovation to enhance empathic communication skills in
medical students. Med Teach 2011;33:663-9.
38. Van Winkle LJ, Fjortoft N, Hojat M. Impact of a workshop
about aging on the empathy scores of pharmacy and medical
students. Am J Pharm Educ 2012;76:9.
39. Bayne HB. Training medical students in empathic communication.
J Spec Group Work 2011;36:316-29.
40. Norfolk T, Birdi K, Walsh D. The role of empathy in establishing
rapport in the consultation: a new model. Med Educ 2007;41:
690-7.
41. Bombeke K, Van Roosbroeck S, De Winter B, Debaene L, Schol
S, Van Hal G, et al. Medical students trained in communication
skills show a decline in patient-centred attitudes: an observational
study comparing two cohorts during clinical clerkships. Patient
Educ Couns 2011;84:310-8.
42. Chatlaong T, Pitanupong J, Wiwattanaworaset P. Sleep Quality
and Burnout Syndrome among Residents in Training at the
Faculty of Medicine, Prince of Songkla University. Siriraj Med
J 2020; 72.307-314.
43. Pitanupong J, Sathaporn K. The prevalence and factors associated
with mistreatment perception among Thai medical students
in a southern medical school. Siriraj Med J. 2019;71.310-7.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














