A Study of Early Parenteral Nutritional Support and Factors Associated with Clinical Outcomes in Major Pediatric Burn Patients
DOI:
https://doi.org/10.33192/Smj.2022.5Keywords:
Early PN, EN, major pediatric burn, nutritional support, treatment outcomesAbstract
Objectives: Adequate nutritional support is one of the challenging treatments of major pediatric burns. Parenteral nutrition (PN) is one of the options to achieve daily caloric goal. Latest nutritional guidelines recommend late PN initiation due to unclear benefit over risk based on the limited data. Our study provides the data of parenteral nutrition within 7 days post admission (early PN) and factors affecting clinical outcomes in major pediatric burn patients.
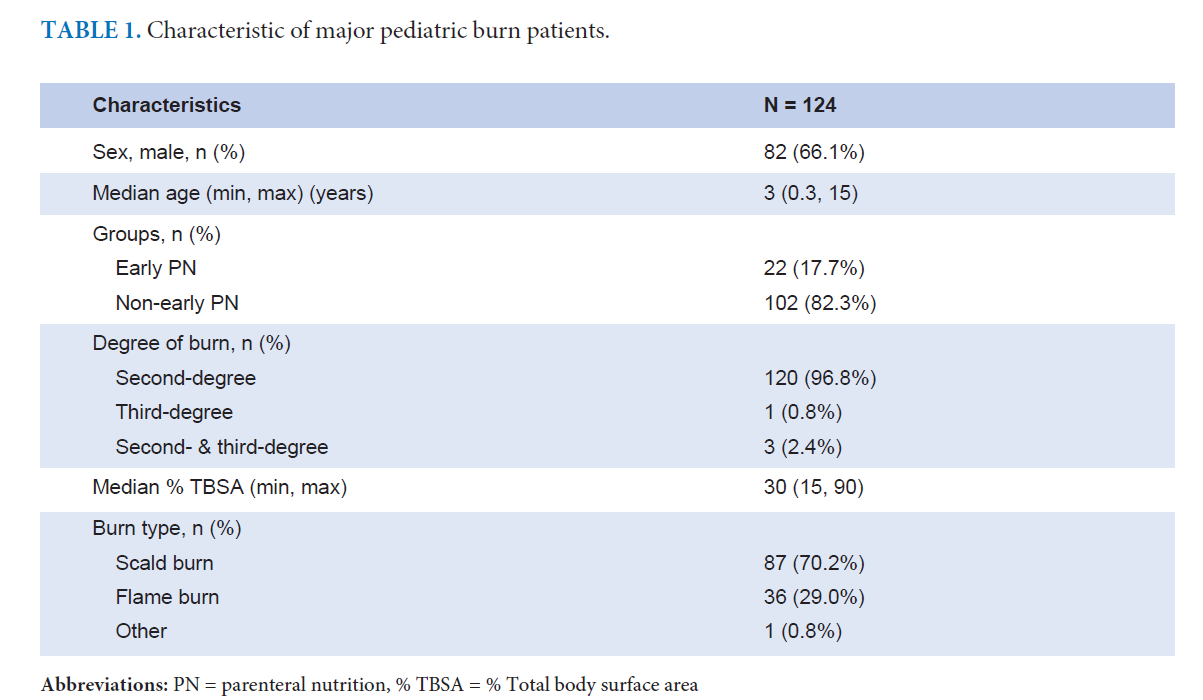
Methods: A retrospective study was conducted regarding pediatric burn patients who had over 15% of their total body surface area (TBSA) with second- or third-degree burns. All the patients were classified as requiring early PN support or non-early PN support.
Results: 124 major pediatric burns were reviewed. Eighty-six patients (65.2%) were male, and the median age was three years (0.3-15 years). Early PN showed no association with length of hospital stay (LOS) (p=0.480) or a 30-day mortality (p=0.529). The children’s age, wound infections, and abdominal distension were the independent associated factors of LOS (p=0.025, 0.001, and 0.003 respectively). Pneumonia and urinary tract infection were independent factors associated with 30-day mortality (p=0.025).
Conclusions: Early PN in acute pediatric burns was not associated with LOS or 30-day mortality. It can be considered as options of nutritional support in acute, major pediatric burns. Effective management of wound infections and abdominal distension may reduce LOS.
References
Pollack MM, Ruttimann UE, Wiley JS. Nutritional depletions in critically ill children: associations with physiologic instability and increased quantity of care. JPEN J Parenter Enteral Nutr. 1985;9(3):309-13.
Mehta NM, Bechard LJ, Cahill N, Wang M, Day A, Duggan CP, et al. Nutritional practices and their relationship to clinical outcomes in critically ill children—an international multicenter cohort study. Crit Care Med. 2012;40(7):2204.
Oosterveld MJ, Van Der Kuip M, De Meer K, De Greef HJ, Gemke RJ. Energy expenditure and balance following pediatric intensive care unit admission: a longitudinal study of critically ill children. Pediatr Crit Care Med. 2006;7(2):147-53.
Joosten KF, Kerklaan D, Verbruggen SC. Nutritional support and the role of the stress response in critically ill children. Curr Opin Clin Nutr Metab Care. 2016;19(3):226-33.
Mehta NM, Skillman HE, Irving SY, Coss-Bu JA, Vermilyea S, Farrington EA, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Pediatric Critically Ill Patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr. 2017;41(5):706-42.
Mehta NM, McAleer D, Hamilton S, Naples E, Leavitt K, Mitchell P, et al. Challenges to optimal enteral nutrition in a multidisciplinary pediatric intensive care unit. JPEN J Parenter Enteral Nutr. 2010;34(1):38-45.
Clark A, Imran J, Madni T, Wolf SE. Nutrition and metabolism in burn patients. Burns & trauma. 2017;5.
Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R, Group PNGW. 1. Guidelines on paediatric parenteral nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005;41:S1-S4.
Fivez T, Kerklaan D, Mesotten D, Verbruggen S, Joosten K, Van den Berghe G. Evidence for the use of parenteral nutrition in the pediatric intensive care unit. Clin Nutr. 2017;36(1):218-23.
Joffe A, Anton N, Lequier L, Vandermeer B, Tjosvold L, Larsen B, et al. Nutritional support for critically ill children. Cochrane Database Syst Rev. 2016;(5):CD005144.
Fivez T, Kerklaan D, Mesotten D, Verbruggen S, Wouters PJ, Vanhorebeek I, et al. Early versus Late Parenteral Nutrition in Critically Ill Children. N Engl J Med. 2016;374(12):1111-22.
Joosten K, Embleton N, Yan W, Senterre T; ESPGHAN/ESPEN/ESPR/CSPEN working group on pediatric parenteral nutrition. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Energy. Clin Nutr. 2018 Dec;37(6 Pt B):2309-14.
Dhopte A, Tiwari VK, Patel P, Bamal R. Epidemiology of pediatric burns and future prevention strategies-a study of 475 patients from a high-volume burn center in North India. Burns Trauma. 2017;5:1.
Keshavarz M, Javanmardi F, Mohammdi AA. A Decade Epidemiological Study of Pediatric Burns in South West of Iran. World J Plast Surg. 2020;9(1):67-72.
Chinaroonchai K, Muangman P, Sirikun J. Dose Acute Kidney Injury Condition Affect Revised BAUX Score in Predicting Mortality in Major Burn Patients? Siriraj Med J. 2019;71:150-8.
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48-79.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al.; Society of Critical Care Medicine; American Society for Parenteral and Enteral Nutrition. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2):159-211.
Taylor BE, McClave SA, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). Crit Care Med. 2016;44(2):390-438.
Sierp EL, Kurmis R, Lange K, Yandell R, Chapman M, Greenwood J, et al. Nutrition and Gastrointestinal Dysmotility in Critically Ill Burn Patients: A Retrospective Observational Study. JPEN J Parenter Enteral Nutr. 2021;45(5):1052-60.
Worthington P, Balint J, Bechtold M, Bingham A, Chan LN, Durfee S, et al. When is parenteral nutrition appropriate? JPEN J Parenter Enteral Nutr. 2017;41(3):324-77.
Sandström R, Drott C, Hyltander A, Arfvidsson B, Scherstén T, Wickström I, et al. The effect of postoperative intravenous feeding (TPN) on outcome following major surgery evaluated in a randomized study. Ann Surg. 1993;217(2):185.
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365(6):506-17.
Chinaroonchai K, Poomsombut P, Muangman P, Sirikun J. Accuracy of Sepsis Criteria of ABA versus CDC for CLABSI Diagnosis in Major Burn Patients, and CLABSI Risk Factors. J Med Assoc Thai 2020;103(Suppl.2):53-9.
Herndon DN, Barrow RE, Stein M, Linares H, Rutan TC, Rutan R, et al. Increased mortality with intravenous supplemental feeding in severely burned patients. J Burn Care Rehabil. 1989;10(4):309–13.
Herndon DN, Stein MD, Rutan TC, Abston S, Linares H. Failure of TPN supplementation to improve liver function, immunity, and mortality in thermally injured patients. J Trauma. 1987;27(2):195–204.
Rosanova MT, Stamboulian D, Lede R. Risk factors for mortality in burn children. Braz J Infect Dis. 2014;18(2):144-9.
Alemayehu S, Afera B, Kidanu K, Belete T. Management Outcome of Burn Injury and Associated Factors among Hospitalized Children at Ayder Referral Hospital, Tigray, Ethiopia Int J Pediatr. 2020;2020:9136256.
Jacobs A, Verlinden I, Vanhorebeek I, Van den Berghe G. Early Supplemental Parenteral Nutrition in Critically Ill Children: An Update. J Clin Med. 2019;8(6):830.
Agbenorku P, Agbenorku M, Fiifi-Yankson PK. Pediatric burns mortality risk factors in a developing country's tertiary burns intensive care unit. Int J Burns Trauma. 2013;3(3):151-8.
Dhopte A, Bamal R, Tiwari VK. A prospective analysis of risk factors for pediatric burn mortality at a tertiary burn center in North India. Burns Trauma. 2017;5:30.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














