Goal-Directed Therapy to Improve Gross Motor Function and the Quality of Life of Children with Cerebral Palsy: A Randomized Controlled Trial
DOI:
https://doi.org/10.33192/Smj.2022.1Keywords:
Cerebral palsy, goal-directed therapy, gross motor function, quality of life, caregiver burdenAbstract
Background: The multiplicity of interventions for the treatment of cerebral palsy (CP) can cause confusion about which are most suited to certain individuals. Hypothesis is that goal-directed therapy (GDT) can guide integrating therapies to improve clinical outcomes compared with conventional therapy (CT).
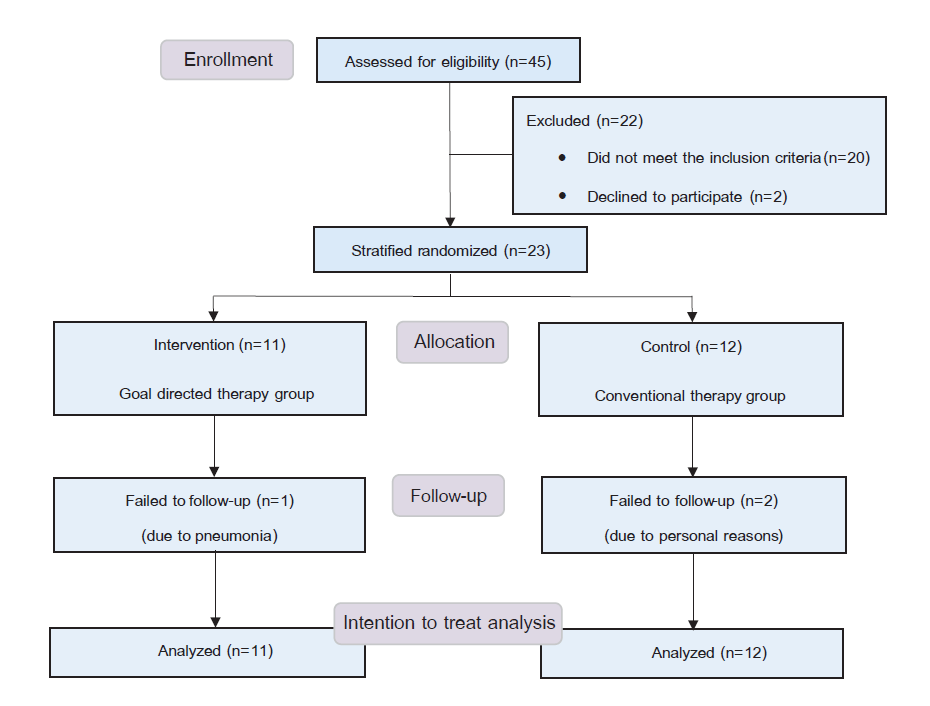
Method: A prospective, assessor-blinded, randomized controlled trial was done with 23 children with CP (mean age, 4 years 4 months old; SD 1y4mo), who were divided into groups according to their level of gross motor function: GDT and CT. Both groups received 12 physiotherapy (PT) sessions and advice on daily home programs. The GDT group additionally had a team meeting to set a specific goal, and PT programs were shaped toward that goal. Assessments were done at baseline and after treatments, using the Thai-version Gross Motor Function Measure (GMFM-66), CP-Quality of Life (CP-QOL), caregiver burden, and home program compliance.
Results: After the treatments, the GDT group showed significant improvements in GMFM-66, CP-QOL, and caregiver burden, while the CT group revealed improvements in caregiver burden and some domains of the GMFM, including sitting and crawling & kneeling. Comparisons between groups found GDT was more effective than CT in improving GMFM-66 and CP-QOL. Home program compliance was higher in the GDT (69%) than the CT group (42%).
Conclusion: GDT demonstrated clear gains for children with CP regarding gross motor function and QOL improvements. Team communication toward a customized goal was crucial, empowering the children and their caregivers to comply with home programs to achieve the set goal.
References
Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55(6): 509-19.
Reddihough DS, Collins KJ. The epidemiology and causes of cerebral palsy. Aust J Physiother. 2003;49(1):7-12.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8-14.
Himmelmann K, Beckung E, Hagberg G, Uvebrant P. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol. 2006;48(6):417-23.
Mohammed FM, Ali SM, Mustafa MA. Quality of life of cerebral palsy patients and their caregivers: A cross sectional study in a rehabilitation center Khartoum-Sudan (2014 - 2015). J Neurosci Rural Pract. 2016;7(3):355-61.
Wimalasundera N, Stevenson VL. Cerebral palsy. Pract Neurol. 2016;0:1-11.
Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, Hines A, et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr Neurol Neurosci Rep. 2020;20(2):3.
Love S, Blair E. The right interventions for each child with cerebral palsy. Dev Med Child Neurol. 2014;56(4):392.
Ketelaar M, Vermeer A, Hart H, van Petegem-van Beek E, Helders PJ. Effects of a functional therapy program on motor abilities of children with cerebral palsy. Phys Ther. 2001;81(9):1534-45.
Ahl LE, Johansson E, Granat T, Carlberg EB. Functional therapy for children with cerebral palsy: an ecological approach. Dev Med Child Neurol. 2005;47(9):613-9.
Law M, Darrah J, Pollock N, King G, Rosenbaum P, Russell D, et al. Family-Centred Functional Therapy for Children with Cerebral PalsyAn Emerging Practice Model. Phys Occup Ther Pediatr. 2009;18:83-102.
Armstrong EL, Boyd RN, Kentish MJ, Carty CP, Horan SA. Effects of a training programme of functional electrical stimulation (FES) powered cycling, recreational cycling and goal-directed exercise training on children with cerebral palsy: a randomised controlled trial protocol. BMJ Open. 2019;9(6):e024881.
Lowing K, Bexelius A, Brogren Carlberg E. Activity focused and goal directed therapy for children with cerebral palsy--do goals make a difference? Disabil Rehabil. 2009;31(22):1808-16.
Lowing K, Bexelius A, Carlberg EB. Goal-directed functional therapy: a longitudinal study on gross motor function in children with cerebral palsy. Disabil Rehabil. 2010;32(11):908-16.
Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet. 2014;383(9924):1240-9.
McConachie H, Huq S, Munir S, Ferdous S, Zaman S, Khan NZ. A randomized controlled trial of alternative modes of service provision to young children with cerebral palsy in Bangladesh. J Pediatr. 2000;137(6):769-76.
Morgan F, Tan BK. Rehabilitation for children with cerebral palsy in rural Cambodia: parental perceptions of family-centred practices. Child Care Health Dev. 2011;37(2):161-7.
Gray L, Ng H, Bartlett D. The gross motor function classification 10 system: an update on impact and clinical utility. Pediatr Phys Ther. 2010;22(3):315-20.
Türker D, Korkem D, Ozal C, Kerem Günel M, Karahan S. The effects of neurodevelopmental (Bobath) therapy based goal directed therapy on gross motor function and functional status of children with cerebral palsy. International Journal of Therapies and Rehabilitation Research. 2015;4(4):9-20.
Hensangvilai K, Yankai A, Angsupaisal M, Intachom R. Reliability in using the Modified Gross Motor Function Measurement-66 Thai version by Physical Therapy students. Journal of medical technology and physical therapy. 2009;21(2):170-85.
Wang HY, Yang YH. Evaluating the responsiveness of 2 versions of the gross motor function measure for children with cerebral palsy. Arch Phys Med Rehabil. 2006;87(1):51-6.
Suwanna K, Prasertsukdee S, Khajornchaikul P. Test-Retest Reliability and Internal Consistency of Cerebral Palsy Quality of Life Questionnaire (Thai version). Thai Journal of Physical Therapy. 2014;36:60-9.
Chumsri S, Chaimongkol N, Sanunruangsak S. Effects of the child caregiver's empowerment promoting program on ability and burden to care for childern with cerebral palsy. The Journal of Faculty of Nursing Burapha University. 2014;22(4):35-46.
Steenbeek D, Ketelaar M, Galama K, Gorter JW. Goal Attainment Scaling in paediatric rehabilitation: a report on the clinical training of an interdisciplinary team. Child Care Health Dev. 2008;34(4): 521-9.
Giessing J, Eichmann B, Steele J, Fisher J. A comparison of low volume ‘high-intensity-training’ and high volume traditional resistance training methods on muscular performance, body composition, and subjective assessments of training. Biol Sport. 2016;33:241-9.
Radaelli R, Fleck SJ, Leite T, Leite RD, Pinto RS, Fernandes L, et al. Dose-response of 1, 3, and 5 sets of resistance exercise on strength, local muscular endurance, and hypertrophy. J Strength Cond Res. 2015;29(5):1349-58.
Argent R, Daly A, Caulfield B. Patient Involvement With Home-Based Exercise Programs: Can Connected Health Interventions Influence Adherence? JMIR Mhealth Uhealth. 2018;6(3):e47.
Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. 2009;23(4):362-70.
Lord C, Rapley T, Marcroft C, Pearse J, Basu A. Determinants of parent-delivered therapy interventions in children with cerebral palsy: A qualitative synthesis and checklist. 2018;44(5):659-69.
Sritipsukho P, Mahasup N. Correlations between gross motor functions and health-related quality of life in Thai children with spastic diplegia. J Med Assoc Thai. 2014;97 Suppl 8:S199-204.
Arnaud C, White-Koning M, Michelsen SI, Parkes J, Parkinson K, Thyen U, et al. Parent-reported quality of life of children with cerebral palsy in Europe. Pediatrics. 2008;121(1):54-64.
Sentenac M, Rapp M, Ehlinger V, Colver A, Thyen U, Arnaud C. Disparity of child/parent-reported quality of life in cerebral palsy persists into adolescence. Dev Med Child Neurol. 2021;63(1): 68-74.
Rapp M, Eisemann N, Arnaud C, Ehlinger V, Fauconnier J, Marcelli M, et al. Predictors of parent-reported quality of life of adolescents with cerebral palsy: A longitudinal study. Res Dev Disabil. 2017;62:259-70.
Uldall P. Chapter 20 - Everyday life and social consequences of cerebral palsy. In: Olivier Dulac ML, Harvey BS, editors. Handbook of Clinical Neurology. Volume 111: Elsevier; 2013. p. 203-7.
Fazzi E, Maraucci I, Torrielli S, Motta F, Lanzi G. Factors predicting the efficacy of botulinum toxin-A treatment of the lower limb in children with cerebral palsy. J Child Neurol. 2005;20(8):661-6.
Funk JF, Panthen A, Bakir MS, Gruschke F, Sarpong A, Wagner C, et al. Predictors for the benefit of selective dorsal rhizotomy. Res Dev Disabil. 2014;37c:127-34.
Published
How to Cite
Issue
Section
License
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














