Knowledge of Stroke and Planned Response among Patients Living with Diabetes Mellitus and Hypertension in a Primary Care Unit
DOI:
https://doi.org/10.33192/Smj.2022.10Keywords:
acute stroke, knowledge, prevention methods, warning symptomsAbstract
Background: Stroke is an important worldwide public health problem. Lack of knowledge in prevention methods, warning symptoms and planned response of acute stroke are associated with a longer prehospital time, which affect the morbidity and mortality of patients.
Objective: The primary objective was to assess knowledge of stroke prevention methods and warning symptoms among patients living with diabetes and/or hypertension. The secondary objectives were to define planned responses when suspecting acute stroke, and identify associated factors with stroke knowledge scores and planned responses.
Materials and Methods: A cross-sectional study was conducted in patients living with diabetes and/or hypertension, who had continuous follow up at the primary care unit of Songklanagarind Hospital. The outcomes of this study were assessed by a questionnaire, which was developed from a literature review.
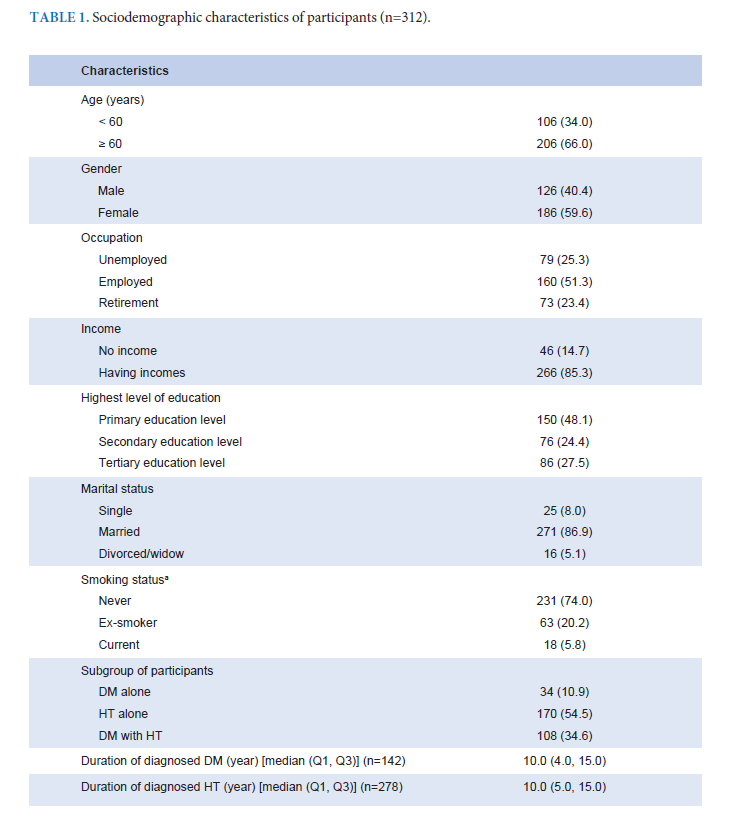
Results: This study included 312 participants. Median age was 64.0 years (Q1, Q3 = 58.0, 71.0), and 59.6% were female. Median score of knowledge of stroke prevention methods were 9, from 12 points (Q1, Q3 = 8, 10), and warning symptoms were 7, from 10 points (Q1, Q3 = 6, 8); with 80.1% of them knowing all 3 warning symptoms, according to the acronym FAST. Only 22.8% of participants would go to the hospital immediately, by calling an ambulance when they experienced symptoms of a suspected acute stroke. Participants who had income had statistically significant higher knowledge of stroke prevention methods; while participants under 60 years of age, who had a longer duration of diagnosed diabetes mellitus were associated with appropriate planned responses when suspecting acute stroke.
Conclusion: Patients living with diabetes mellitus and hypertension, who are at a high risk for developing cardiovascular diseases, still do not have enough knowledge about acute stroke and had little concern about developing a stroke; especially the elderly and those with a short duration of having been diagnosed with diabetes mellitus.
References
Benjamin EJ, Muntner P, Alonso A, Bittercourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: summary a report from the American Heart Association. Circulation 2020;139:e354-88.
Gorelik PB. The global burden of stroke: persistent and disabling. Lancet Neurol 2019;18:418-7.
American stroke association. Stroke: risk factors, symptoms and preventions [Internet]. 2019[cited 2019 October 10].
Available from: https://www.stroke.org/en/about-stroke/strokerisk- factors
Muengtaweepongsa S, Hunghok W, Harnirattisai T. Poor recognition of prompted treatment seeking even with good knowledge of stroke warning signs contribute to delayed arrival of acute ischemic stroke patients in Thailand. J Stroke Cerebrovasc Dis 2014;23:948-52.
Hankey JG. Stroke. Lancet 2017;389:641-54.
Romano JG. Thrombolysis in Maxico: current status and opportunities. Revista Mexicana de Neurociencia 2019;20: 208-9.
Ratanakorn D, Keandoungchun J, Sittichanbuncha Y, Laothamatas J, Tegeler CH. Stroke fast track reduces time delay to neuroimaging
and increases use of thrombolysis in an academic medical center in Thailand. J Neuroimaging 2012 ;22:53-7.
Lekpet J, Wuthisuthimethawee P, Vasinanukorn P. Prehospital time and emergency department time for acute ischemic stroke care at Songklanagarind hospital. Songkla Med J 2009;27:206-12.
Fladt J, Meier N, Thilemann S, Polymeris A, Traenka C, Seiffge DJ, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc 2019;8:e013101.
Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, et al. Factors associated with prehospital delays in the presentation of acute stroke in Urban China. Stroke 2012;43:362-70.
Hong ES, Kim SH, Kim WY, Ahn R, Hong JS. Factors associated with prehospital delay in acute stroke. Emerg Med J 2011;28: 790-3.
Ching S, Chia Yc, Chew BN, Soo MJ, Lim HM, Wan Sulaiman WA, et al. Knowledge on the action to be taken and recognition of symptoms of stroke in a community: findings from the May measurement month 2017 blood pressure screening programme in Malaysia. BMC Public Health 2019;19:1-12.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. AHA journals 2019; 50: e344–e418.
Suwanwela NC, Chutinet A, Kijpaisalratana N. Thrombolytic treatment in Thailand. J Stroke Med 2018;1:41-4.
American stroke association. Stroke symptoms [Internet]. 2021[cited 2021 Feb 3]. Available from: https://www.stroke.org/en/about-stroke/stroke-symptoms
Kleindorfer DO, Miller R, Moomaw CJ, Alwell K, Broderick JP, Khoury J, et al. Designing a message for public education regarding stroke: does FAST capture enough stroke? AHAjournal 2007;38:2864-8.
American stroke association, Stroke risk factors you can control, treat and improve [Internet]. 2018[cited 2019 July 20]. Available
from: https://www.stroke.org/en/about-stroke/stroke-riskfactors/stroke-risk-factors-you-can-control-treat-and-improve 84 Volume 74, No.2: 2022 Siriraj Medical Journal https://he02.tci-thaijo.org/index.php/sirirajmedj/index
Nakibuuka J, Sajatovic M, Katabira E, Ddumba E, Byakika-Tusiime J, Furlan AJ. Knowledge and perception of stroke: a populationbased
survey in Uganda. ISRN Stroke 2014:1-7.
Dossi DE, Hawkes MA, Pujol-Lereis VA, Povedano GP, Rodriguez-Lucci F, Farez MF, et al. A population-based survey of stroke knowledge in Argentina: the SIFHON study. Neuroepidemiology 2019:1-9
Han CH, Kim H, Lee S, Chung JH. Knowledge and poor understanding factors of stroke and heart attack symptoms. Int. J. Environ. Res. Public Health 2019;16:1-11.
Hickey A, Mellon L, Williams D, Shelly E, Conroy R. Does stroke health promotion increase awareness of appropriate behavioral response? Impact of the face, arm, speech and time (FAST) campaign on population knowledge of stroke risk factors, warning signs and emergency response. Eur Stroke J 2018;3:117-25.
Li RC, Xu WD, Lei YL, Bao T, Yang HW, Huang WX, et al. The risk of stroke and associated risk factors in a health examination population: a cross-sectional study. Medicine 2019;98;1-7.
Saengsuwan J, Suangpho P, Tiamkao S. Knowledge of Stroke Risk Factors and Warning Signs in Patients with Recurrent Stroke or Recurrent Transient Ischaemic Attack in Thailand. Neurol Res Int 2017;2017:8215726.
Centers for Disease Control and Prevention. Glossary [Internet]. National Center for Health Statistics;2021 [ cited 2020 Jan 23]. Available from: https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm
Wattanapan P, Singhpoo K, Charerntanyarak L, Nualnert N, Sangsuwan J, Ngamroop R, et al. Factors influencing stroke knowledge among Thai rural population. J Med Assoc Thai 2018; 101:S83-8.
Hooser JV, Rouse KL, Meyer ML, Siegler AM, Freuhauf BM, Balance EH, et al. Knowledge of heart attack and stroke symptoms among US native American adults: a cross-sectional populationbased study analyzing a multi-year BRFSS database. BMC Public Health 2020;20:1-10.
Krishnamurthi RV, Barker-Collo S, Barber PA, Tippet L, Dalrymple-Alford JC,Tunnage B, et al. Community knowledge and awareness of stroke in New Zealand. Journal of stroke and cerebrovascular disease 2019;10:1-9.
Abate AT, Bayu N, Mariam TG. Hypertensive Patients’ Knowledge of Risk Factors and Warning Signs of Stroke at Felege Hiwot Referral Hospital, Northwest Ethiopia: a cross-sectional study. Neurol Res Int 2019;2019:8570428.
Dar NZ, Khan SA, Ahmad A, Maqsood S. Awareness of stroke and health-seeking practice among hypertensive patients in a tertiary care hospital: a cross-sectional survey. Cureus 2019;11:1-15.
Arisegi SA, Awosan KJ, Oche MO, Sabir AA, Ibrahim MT. Knowledge and practices related to stroke prevention among hypertensive and diabetic patients attending Specialist Hospital, Sokoto, Nigeria. Pan Afr Med J 2018;29:63.
Ananchaisarp T., Rungruang S., Theerakulpisut S., Kamsakul P., Nilbupha N., Chansawangphop N., et al. Usage of herbal medicines among the elderly in a primary care unit in Hat Yai, Songkhla province, Thailand. Asian Biomed 2021;15:35-42.
Peltzer K, Pengpid S. The use of herbal medicines among chronic disease patients in Thailand: a cross-sectional survey. J Multidiscip
Healthc 2019;12:573-81.
Kanjanahattakij N, Kwankao P, Vathesatogkit P, Thongmung N, Gleebbua Y, Sritara P, et al. Herbal or traditional medicine consumption in a Thai worker population: pattern of use and therapeutic control in chronic disease. BMC Complement Altern Med 2019;19:1-9.
Kaddumukasa M, Kayima J, Nakibuuka J, Mugenyi L, Ddumba E, Blixen C, et al. A cross-sectional population survey on stroke knowledge and attitudes in Greater Kampala, Uganda. Cogent Med 2017;4:1-12.
Duque AS, Fernades L, Correia AF, Calvinho I, Cardoso G, Pinto M et al. Awareness of stroke risk factors and warning signs and attitude to acute stroke. iMedPub J 2015;8:1-18.
Mano H. Perceived stroke warning signs among hypertensive patients, Long hospital, Ohrae province. Chiang Mai: Chiang Mai University; 2009. p.1-92.
Mould-Millman NK, Rominski SD, Bogus J, Ginde AA, Zakariah AN, Boatemaah CA, Yancey AH, Akoriyea SK, Campbell TB. Barriers to accessing emergency medical services in Accra, Ghana: development of a survey instrument and initial application in Ghana. Glob Health Sci Pract 2015;3:577-90.
Sultan M, Abebe Y, Tsadik AW, Ababa A, Yesus AG, Mould-Millman NK. Trends and barriers of emergency medical service use in Addis Ababa; Ethiopia. BMC Emerg Med 2019;19:28.
Patel A, Fang J, Gillespie C, Odom E, King AC, Luncheon C, et al. Awareness of stroke signs and symptoms and calling 9-1-1 among US adults: National Health interview survey, 2009 and 2014. Prev Chronic Dis 2019;16:180564.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














