Detection of Postoperative Cognitive Dysfunction by Telemedicine Among Octogenarian Patients Who Underwent Minor Elective Surgery; Prospective Cohort Study
DOI:
https://doi.org/10.33192/Smj.2022.16Keywords:
Anesthesia, geriatrics, postoperative cognitive dysfunction, RUDAS-Thai, telemedicineAbstract
Objective: Postoperative cognitive dysfunction (POCD) is associated with permanent disability, increased mortality, and diminished quality of life. The incidence of acute POCD among geriatric patients who have undergone minor surgery is uncertain because they are typically discharged before acute POCD is detected. Owing to the efficient postoperative care that can be provided, telemedicine is an attractive tool to investigate POCD. The primary objective of our research was to explore the incidence of acute POCD, while its secondary objective was to describe the consequences of POCD on functional recovery and quality of life.
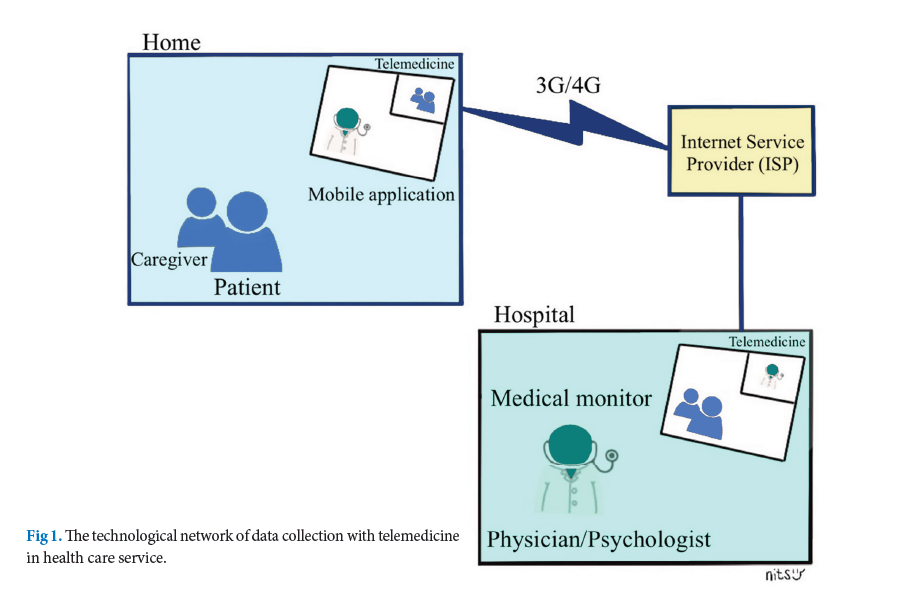
Materials and Methods: This prospective cohort study enrolled patients aged ≥ 80 years and scheduled for minor elective surgery. During pre-anesthetic visits, we installed a telecommunications program on the patients’ smartphones. Assessments of cognitive and other functions were performed preoperatively and 1 week postoperatively via telemedicine.
Results: Forty octogenarian patients undergoing minor surgery were included in the final analysis. The acute-POCD incidence was 10% (95% CI 4.79-18.39). Recall memory was the main cognitive domain impaired after the procedures. Nevertheless, there were no significant differences in the functional recovery and quality of life of the POCD and non-POCD patients.
Conclusion: The acute-POCD patients demonstrated minor symptoms that were unrelated to delayed postoperative functional recovery or decreased quality of life.
References
Yang R, Wolfson M, Lewis MC. Unique Aspects of the Elderly Surgical Population: An Anesthesiologist’s Perspective. Geriatr Orthop Surg Rehabil. 2011;2(2):56-64.
Wang W, Wang Y, Wu H, Lei L, Xu S, Shen X, et al. Postoperative cognitive dysfunction: current developments in mechanism and prevention. Med Sci Monit. 2014;20:1908-12.
Pappa M, Theodosiadis N, Tsounis A, Sarafis P. Pathogenesis and treatment of post-operative cognitive dysfunction. Electron Physician. 2017;9(2):3768-75.
Rundshagen I. Postoperative cognitive dysfunction. Dtsch Arztebl Int. 2014;111(8):119-25.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. 1998; 351(9106):857-61.
Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110(3):548-55.
Tsai TL, Sands LP, Leung JM. An Update on Postoperative Cognitive Dysfunction. Adv Anesth. 2010;28(1):269-84.
Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, et al. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiol Scand. 2003;47(10):1204-10.
Gunter RL, Chouinard S, Fernandes-Taylor S, Wiseman JT, Clarkson S, Bennett K, et al. Current Use of Telemedicine for Post-Discharge Surgical Care: A Systematic Review. J Am Coll Surg. 2016;222(5):915-27.
Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823-7.
Ian smith, Mark A. Skues, and Beverly et, al. Ambulatory (outpatient) anesthesia, chapter 72. Miller’s Anesthesia, ninth edition, 2020.
Storey JE, Rowland JT, Basic D, Conforti DA, Dickson HG. The Rowland Universal Dementia Assessment Scale (RUDAS): a multicultural cognitive assessment scale. Int Psychogeriatr. 2004;16(1):13-31.
Limpawattana P, Tiamkao S, Sawanyawisuth K, Thinkhamrop B. Can Rowland Universal Dementia Assessment Scale (RUDAS) replace Mini-mental State Examination (MMSE) for dementia screening in a Thai geriatric outpatient setting? Am J Alzheimers Dis Other Demen. 2012;27(4):254-9.
Wong L, Martin-Khan M, Rowland J, Varghese P, Gray LC. The Rowland Universal Dementia Assessment Scale (RUDAS) as a reliable screening tool for dementia when administered via videoconferencing in elderly post-acute hospital patients. J Telemed Telecare. 2012;18(3):176-9. Suesat et al. https://he02.tci-thaijo.org/index.php/sirirajmedj/index Volume 74, No.2: 2022 Siriraj Medical Journal 133
Original Article SMJ
Hensel A, Angermeyer MC, Riedel-Heller SG. Measuring cognitive change in older adults: reliable change indices for the Mini-Mental State Examination. J Neurol Neurosurg Psychiatry. 2007;78(12):1298-303.
Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64-7.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727-36.
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-9.
Elashoff JD. nQuery Advisor Version 7.0 User’s Guide. Cork, Ireland, Statistical Solutions Ltd 2007.
Safavynia SA, Goldstein PA. The Role of Neuroinflammation in Postoperative Cognitive Dysfunction: Moving From Hypothesis to Treatment. Front Psychiatry. 2018;9:752.
Lima-Silva TB, Yassuda MS. The relationship between memory complaints and age in normal aging. Dement Neuropsychol. 2009;
(2):94-100.
Philp DJ, Korgaonkar MS, Grieve SM. Thalamic volume and thalamo-cortical white matter tracts correlate with motor and verbal memory performance. Neuroimage. 2014;91:77-83.
Fama R, Sullivan EV. Thalamic structures and associated cognitive functions: Relations with age and aging. Neurosci Biobehav Rev. 2015;54:29-37.
Glumac S, Kardum G, Sodic L, Supe-Domic D, Karanovic N. Effects of dexamethasone on early cognitive decline after cardiac surgery: A randomised controlled trial. Eur J Anaesthesiol.2017;34(11):776-84.
Phillips-Bute B, Mathew JP, Blumenthal JA, Grocott HP, Laskowitz DT, Jones RH, et al. Association of neurocognitive function and quality of life 1 year after coronary artery bypass graft (CABG) surgery. Psychosom Med. 2006;68(3):369-75.
Bárrios H, Narciso S, Guerreiro M, Maroco J, Logsdon R, de Mendonça A. Quality of life in patients with mild cognitive impairment. Aging Ment Health. 2013;17(3):287-92.
Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, et al. Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: a systematic review and meta-analysis. BMC Public Health. 2019;19(1):832.
Steinmetz J, Siersma V, Kessing LV, Rasmussen LS. Is postoperative cognitive dysfunction a risk factor for dementia? A cohort follow-up study. Br J Anaesth. 2013;110 Suppl 1:i92-7.
Rios G. eHealth Literacy and Older Adults: A Review of Literature. Topics in Geriatric Rehabilitation 2013;29:116–125.
Leung JM, Sands LP, Mullen EA, Wang Y, Vaurio L. Are preoperative depressive symptoms associated with postoperative
delirium in geriatric surgical patients? J Gerontol A Biol Sci Med Sci. 2005;60(12):1563-8.
Jakobsson E, Nygård L, Kottorp A, Malinowsky C. Experiences from using eHealth in contact with health care among older
adults with cognitive impairment. Scand J Caring Sci. 2019;33(2): 380-9.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














