The Prevalence and Risk Factors of Storage Urinary Symptoms in Symptomatic COVID-19 Patients Who were Treated in Cohort Ward and Field Hospital
DOI:
https://doi.org/10.33192/Smj.2022.17Keywords:
Storage symptoms, COVID-19, SARS-CoV-2 virus, viral cystitisAbstract
Objective: The primary aim of this study was to focus on the prevalence of storage symptoms in COVID-19 patients and the factors associated with those symptoms.
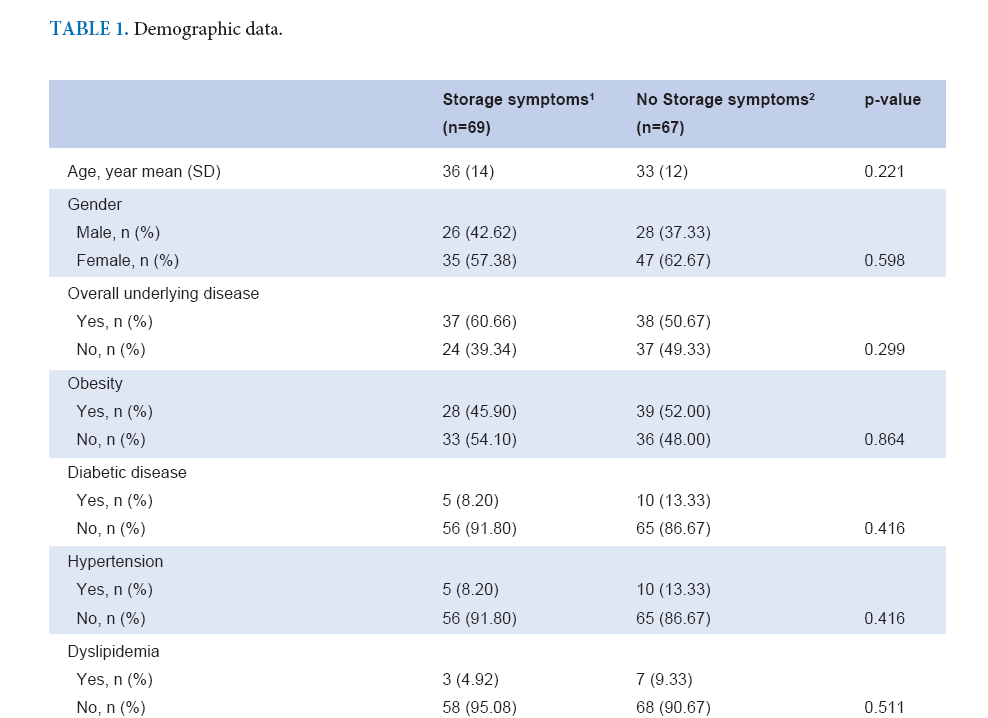
Material and Methods: We collected the data of COVID-19 patients who were admitted to the cohort ward, ICU and field hospital of Thammasat University Hospital, Thailand, between May and June 2021. Patients answered online survey questions and undertook urinalysis by urine dipstick test. The online survey questions related to symptoms of COVID-19 infection, number of daytime voiding, nocturia, frequency and urgency symptom during COVID-19 infection, OABSS and ICIQ-LUTS in the part of storage symptoms subscale.
Results: There were 136 COVID-19 patients who met with the eligible criteria and were willing to participate in the study. Patients who had storage symptoms totaled 61 (44.85%) and had average daytime frequency, nocturia and proportion of urgency higher than no storage symptom group (5.9 VS 3.8, 2.0 VS 1.0 and 67.21% VS 6.67% (p-value <0.001), respectively). The OABSS and ICIQ storage subscale in the storage symptoms group were higher than normal group, 3.2 VS 0.9 and 4.5 VS 1.7 (p-value < 0.001), respectively.
Conclusion: Our study demonstrated that the SARS-CoV-2 virus infection is associated with abnormal storage
symptoms which include frequency, urgency and nocturia. The storage symptoms may be associated with the
severity of COVID-19 disease.
References
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. Jama. 2020; 324(8):782-93.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20.
Sun J, Zhu A, Li H, Zheng K, Zhuang Z, Chen Z, et al. Isolation of infectious SARS-CoV-2 from urine of a COVID-19 patient. Emerg Microbes Infect. 2020;9(1):991-3.
Mumm JN, Osterman A, Ruzicka M, Stihl C, Vilsmaier T, Munker D, et al. Urinary Frequency as a Possibly Overlooked Symptom in COVID-19 Patients: Does SARS-CoV-2 Cause Viral Cystitis? Eur Urol. 2020;78(4):624-8.
Kaya Y, Kaya C, Kartal T, Tahta T, Tokgöz VY. Could LUTS be early symptoms of COVID-19. Int J Clin Pract. 2021;75(3):e13850.
Swatesutipun V, Tangpaitoon T. Lower Urinary Tract Symptoms (LUTS) Related to COVID-19: Review Article. J Med Assoc Thai. 2021;104:1045-9.
Kashi AH, De la Rosette J, Amini E, Abdi H, Fallah-Karkan M, Vaezjalali M. Urinary Viral Shedding of COVID-19 and its Clinical Associations: A Systematic Review and Meta-analysis of Observational Studies. Urol J. 2020;17(5):433-41.
Roshandel MR, Nateqi M, Lak R, Aavani P, Sari Motlagh R, S FS, et al. Diagnostic and methodological evaluation of studies on the urinary shedding of SARS-CoV-2, compared to stool and serum: A systematic review and meta-analysis. Cell Mol Biol (Noisy-le-grand). 2020;66(6):148-56.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-8.
Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020;14(2):185-92.
Lamb LE, Dhar N, Timar R, Wills M, Dhar S, Chancellor MB. COVID-19 inflammation results in urine cytokine elevation and causes COVID-19 associated cystitis (CAC). Med Hypotheses. 2020;145:110375.
Welk B, Richard L, Braschi E, Averbeck MA. Is coronavirus disease 2019 associated with indicators of long-term bladder dysfunction?
Neurourol Urodyn. 2021;40(5):1200-6.
Liu R, Ma Q, Han H, Su H, Liu F, Wu K, et al. The value of urine biochemical parameters in the prediction of the severity of coronavirus disease 2019. Clin Chem Lab Med. 2020;58(7):1121-4.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














