Factors Influencing the Quality of Life and Nutritional Status of 0-2 Years Old Children
DOI:
https://doi.org/10.33192/Smj.2022.18Keywords:
Children aged 0-2, quality of life, nutritional status, child-rearing practice, access to healthcareAbstract
Objective: To investigate the effects of children factors, family factors, and access to healthcare services on children’s quality of life as perceived by caregivers and nutritional status of 0 to 2 years old children.
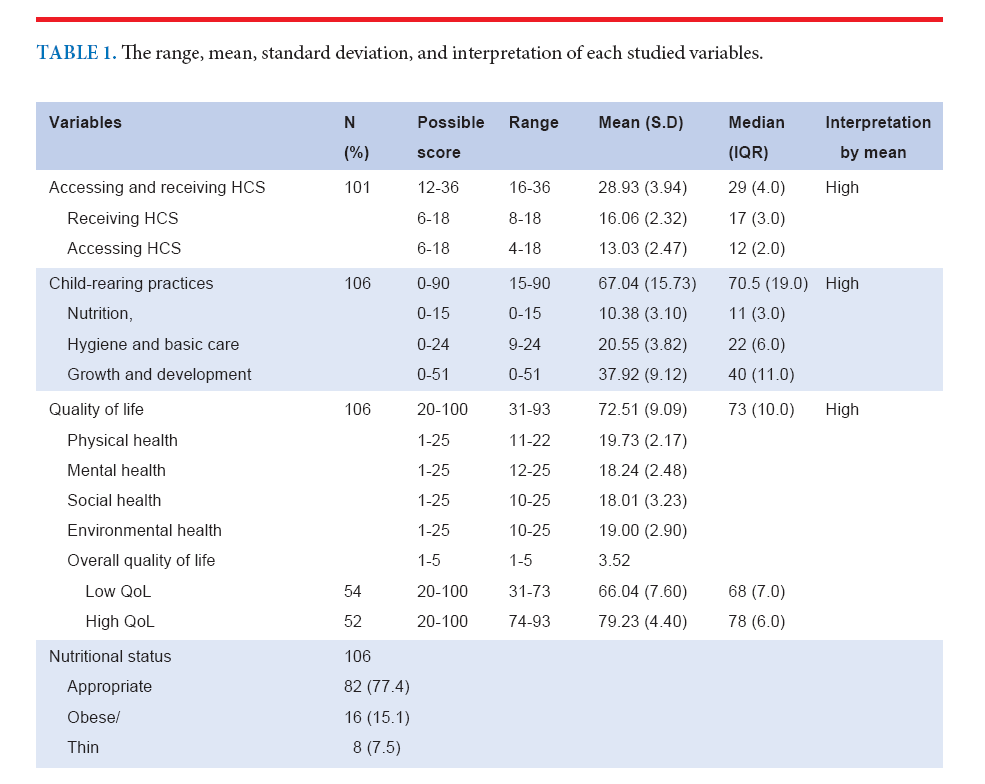
Materials and Methods: This study employed predictive design. The sample group consisted of 106 caregivers with children aged 0 to 2 years old from five subdistricts in one province in Central region in Thailand. The research instruments included the Demographic Data of Parents and Children Questionnaire; the Access to Healthcare Services Questionnaire; the Child-Rearing Practices Questionnaire; the Quality of Life of 0-2-year-old Children Questionnaire. The data were analyzed by using the Chi-square, Fisher’s exact test, and multivariate logistic regression.
Results: Logistic regression model accounted for 34 % of variance in children’s quality of life (Nagelkerke R2= 0.34) and 35.3% of variance in their nutritional status (Nagelkerke R2=.35). Factors predicting the QoL of children were the maternal age (OR=4.75; 95%CI = 1.16, 19.45, p < .05), and the child-rearing practices (OR=5.68; 95%CI = 1.97, 16.40, p < .05). Factors predicting nutritional status were maternal age (OR=0.088; 95%CI = 0.01, 0.79; OR=0.225; 95%CI=0.02, 2.34, p < .05), and child-rearing practices (OR=7.84; 95%CI = 1.93, 31.84, p < .05). Finally, access to healthcare services had a significant association with QoL of children (χ2 = 9.632, p < .05).
Conclusion: Healthcare personnel should improve children’s quality of life and nutritional status by organizing programs to promote child-rearing practices and facilitating parents for accessibility to healthcare services.
References
Aekplakorn W. Thai national health examination survey, NHES V. Health System Research Institute (HSRI). [Internet]. 2014 [cited 16 Nov 2020]. Available from: https://www.hiso.or.th/hiso/picture/reportHealth/report/thai2014kid.pdf
National Statistical Office and UNICEF. Thailand Multiple Indicator Cluster Survey 2019. Survey Finding Report. [Internet]. 2019 [cited 16 Nov 2020]. Available from: https://www.unicef.org/thailand/reports/thailand-multiple-indicator-clustersurvey-2019
World Health Organization. Malnutrition. [Internet]. 2021 [cited 24 Sep 2021]. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition
Ubesie AC, Ibeziakor NS. High burden of protein-energy malnutrition in Nigeria: beyond the health care setting. Ann Med Health Sci Res. 2012; 2(1):66–9. PMID:23209994
World Health Organization. Programme on mental health: WHOQOL user manual 2012. Division of Mental Health and Prevention of Substance Abuse. WHO/HIS/HSI Rev.2012.03;2012.
Varni JW, Limbers CA, Neighbors K, Schulz K, Lieu JE, Heffer RW, et al. The PedsQL™ Infant Scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual Life Res. 2011 Feb;20(1):45–55. DOI: 10.1007/s11136-010-9730-5.
Wallander JL, Koot HM. Quality of life in children: A critical Rungamornrat et al. https://he02.tci-thaijo.org/index.php/sirirajmedj/index Volume 74, No.3: 2022 Siriraj Medical Journal 151 Original Article SMJ examination of concepts, approaches, issues, and future directions.
Clin Psychol Rev. 2016;45:131-43. DOI: 10.1016/j.cpr.2015.11.007.
Solans M, Pane S, Estrada M, Serra-Sutton V, Berra S, Herdman M, et al. Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease-specific instruments. Value Health. 2008;11(4):742-64. DOI: 10.1111/j.1524-
2007.00293.x.
Hayeese W, Sap-In N, Wangsawat T, Chaimongkol N.Influencing factors of quality of life of Muslim preterm infants in the three southernmost provinces. J Fac Nurs Burapha University. 2015;23(3):26-40.
Schepers SA, van Oers HA, Maurice-Stam H, Verhaal CM, Grootenhuis MA, Haverman L. Health related quality of life in Dutch infants, toddlers, and young children. Health Qual Life Outcome. 2017; 15(1):81. DOI: 10.1186/s12955-017-0654-4.
Mahatnirunkul S, Tantiphiwatthanasakun W, Pumpaisalchai W, Wongsuwan K, Pornmanajirangul. Quality of life indicators of The WHO (Thai version). [Internet]. 2020. [Cited 2020 October 19]. Available from: https://www.dmh.go.th/test/download/files/whoqol.pdf.
Fekadu Y, Mesfin A, Haile D, Stoeker BJ. Factors associated with nutritional status of infant and young children in Somali Region, Ethiopia; a cross sectional study. BMC Public Health. 2015;15:846. DOI: 10.1186/s12889-015-2190-7.
Noijeen N, Rungamornrat S, Srichantaranit A. Predictive Factors of Growth Among Preterm Migrant Children in Kanchanaburi Province, Thailand. J Popul Soc. 2021;29:401-15.
Kalu RE, Etim KD. Factors associated with malnutrition among under-five children in developing countries: a review. Glob. J. Pure Appl. 2018;24:69-74. DOI:10.4314/gjpas.v24i1.8.
Ouyang N, Lu X, Cai R, Liu M, Liu K. Nutritional screening and assessment, and quality of life in children with cancer: a cross-sectional study in mainland China. J Pediatric Nurs. 2021;57:99-105. DOI:https://doi.org/10.1016/j.pedn.2020.07.013.
Kourkoutas E, Giorgiadi M, Plexousakis GS. Quality of life of children with chronic illnesses: A Review of the Literature. Procedia Soc Behav Sci. 2010;2(2):4763-7.
Cribb VL, Jones LR, Rogers IS, Ness AR, Emmett PM. Is maternal education level associated with diet in 10-year-old children? Public Health Nutr. 2011 Nov;14(11):2037-48. PMID: 21414248
Joel A, Victoria NA, Eunice U, Evans P. Assessment of Nutritional Status of Children 0 – 2 years and Associated Factors in Some Selected Primary Health Centres in Osun State. Journal of Positive Psychology and Counselling. 2020;20:15-27.
Gladstone M, Phuka J, Mirdamadi S, Chitimbe F, Koenraads M, Maketa J. The care, stimulation and nutrition of children from 0-2 in Malawi-perspective form caregiver; “Who’s holding the baby?”. 2018; 13(6):e0199757. Available from: https://doi.org/10.1371/journal.pone.0199757
Tangcharoensathien V, Witthayapipopsakul W, Panichkriangkrai W, Patcharanarumol W, Mills A. Health systems development in
Thailand: a solid platform for successful implementation of universal health coverage. Lancet. 2018;391:1205–23.
Seid M, Varni JW, Cummings L, Schonlau M. The impact of realized access to care on health-related quality of life: a two-year prospective cohort study of children in the California State Children’s Health Insurance Program. J Pediatr. 2006;149(3):354-61. DOI:10.1016/j.jpeds.2006.04.024.
Cheak-Zamora N, Farmer JE. The Impact of the Medical Home on Access to Care for Children with Autism Spectrum Disorders. J Autism Dev Disord. 2015;45:636-44. DOI:10.1007/s10803-014-2218-3.
The Center for the Protection of Children’s Right Foundation. Tools development for minimum standard of child rearing in accordance to the Child Protection Act 2003. The Ministry of Social Development and Human Security; 2003.
Gubbels JS, Stessen K, de Kolk IV, de Vries N K. Thijs C, Kremers S. Energy balance-related parenting and childcare practices: The importance of mesosystem consistency. PLOS ONE.2018. DOI.org/10.1371/journal.pone.0203689
Monitoring the situation of children and women: Multiple Indicator Cluster Survey 2015-2016. [Internet]. [Cited 2020 Feb 20]. Available from: https://www.unicef.org/thailand/media/201/file/Thailand%20MICS%202015-2016%20(full%20report).pdf
Rungamornrat S, Nookomg A, Kraimongkol N, Puttisatien R. Implementation of Nutritional Promotion Guidelines for Preschool Children with Overweight in a Childcare Centre. Thai J Nurs Council. 2017;32(4):120–33.
World Health Organization. Obesity and overweight. [internet]. [Cited 2020 Mar 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Electronic Transactions Development Agency, Ministry of,Digital Economy and Society. (2020). Thailand Internet User Behavior 2019. [Cited 2021 April 23]. Available from: https://www.etda.or.th/th/NEWS/ETDA-Revealed-Thailand-Internet-User-Behavior-2019.aspx
Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012 Jun;24(3):176-88. PMID:22724639
Lei L. The impact of community context on children’s health and nutritional status in China. Soc Sci Med. 2017; 179:172–81.PMID:28285233
Haszard JJ, Russell CG, Byrne RA, Taylor RW, Campbell KJ. Early maternal feeding practices: associations with overweight later in childhood. Appetite. 2019;132(1):91-6. PMID:30308224
Zevulun D, Post WJ, Zijlstra AE, Kalverboer ME, Knorth EJ. The Best Interests of the Child from Different Cultural Perspectives: Factors Influencing Judgements of the Quality of Child-Rearing Environment and Construct Validity of the Best Interests of the Child-Questionnaire (BIC-Q) in Kosovo and Albania. Child Indic Res. 2019;12(1):331-51.
Gomes AM, Riberi RF. Parental practice and beliefs on motor development in the first year of life. Fisioter Mov. 2017;30(4):769-79.
Yunus KR, Dahlan NA. Child-rearing practices and socioeconomic status: possible implications for children’s educational outcomes. Procedia Soc Behav Sci. 2013;90:251-9.
Garcia-Subirats I, Vargas I, Mogollón-Pérez AS, De Paepe P, da Silva MR, Unger JP, et al. Inequities in access to health care in different health systems: a study in municipalities of central Colombia and north-eastern Brazil. Int J Equity Health. 2014;13:10. https://doi.org/10.1186/1475-9276-13-10 PMID:24479581
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














