Survival of Non-Small Cell Lung Cancer Patients with Unexpected N2 after Complete Resection: Role of Aggressive Invasive Mediastinal Staging should be Considered
DOI:
https://doi.org/10.33192/Smj.2022.20Keywords:
N2 disease, Unexpected N2, Non-small lung cancer (NSCLC), Invasive mediastinal staging (IMS), Stage 3A NSCLCAbstract
Objective: Mediastinal lymph node (N2) metastasis is one of the poor prognostic factors in non-small cell lung cancer patients (NSCLC). However, the accuracy of mediastinal lymph node staging in real practice is uncertain and inadequate. Consequently, the aim of this study was to determine the survival of NSCLC patients with clinically non-suspicious mediastinal lymph node metastases who underwent complete resection but were pathologically confirmed as having N2 metastases (unexpected N2).
Materials and Methods: A retrospective review was performed of all pathology-proven N2 metastases NSCLC patients who underwent curative surgical resection from January 2007 to December 2016. A total of 158 patients were initially included in the study. After the exclusions (known N2, small cell carcinomas, neuroendocrine tumor), 125 unexpected N2 patients who underwent complete resection were analyzed. Survival analysis was determined using the Kaplan–Meier method and multivariate analysis was determined using the Cox regression method.
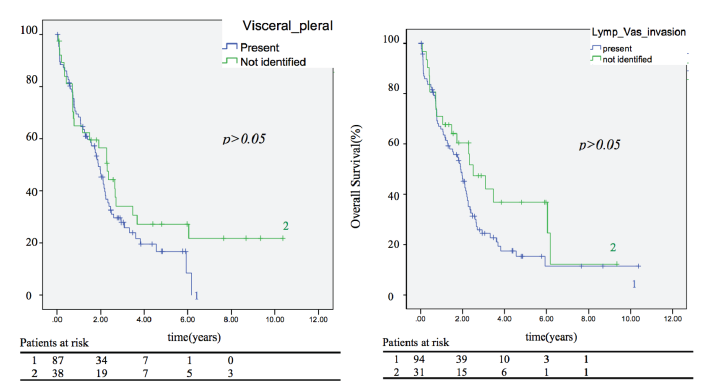
Results: The overall 2-year, 3-year, and 5-year survival rates were 40%, 24%, and 20% respectively. Complete resection was achieved in all patients. Invasive mediastinal staging (IMS) was performed in 47 patients (37.6%), by endobronchial ultrasonography (EBUS) in 46 (36.8%) patients (82.6% negative and 17.4% inadequate tissue) while only 1 patient underwent mediastinoscopy. The factors affecting the survival rate upon comparison were the histology type (p=0.019), differentiate characteristics (p=0.004), adjuvant therapy (p=0.011), and presence of distant metastasis by postoperative re-staging (p=0.003). The independent predictive factors for survival were
chemo-radiation therapy (odds ratio 0.367, 95% confidence interval 0.176–0.766) and distant metastasis (odds ratio 2.280, 95% confidence interval 1.334–3.897). However, a small size, periphery lesion, T staging, and number of N2 lesions were not significant factors.
Conclusion: The survival rate of unexpected N2 patients was low despite complete resection being achieved in these patients. Adjuvant therapy seemed to improve survival for those with unexpected N2 metastasis as it is a systemic disease. However, not all patients received IMS, which was mostly done by EBUS and which had a high false negative, leading to underestimating the staging. Other modalities, such as cervical mediastinoscopy, videoassisted mediastinoscopic lymphadenectomy (VAMLA) or open biopsy should be considered for the adequate evaluation of N2 metastasis, nonetheless further study is still needed.
References
Friedel G, Steger V, Kyriss T, Zoller J, Toomes H. Prognosis in N2 NSCLC. Lung Cancer 2004;45(Suppl):45-53.
Goya T, Asamura H, Yoshimura H, Kato H, Shimokata K, Tsuchiya R, et al. Prognosis of 6644 resected non-small cell lung cancers in Japan: a Japanese lung cancer registry study. Lung Cancer 2005;50:227–34.
Kang CH, Ra YJ, Kim YT, Jheon SH, Sung SW, Kim JH. The impact of multiple metastatic nodal stations on survival in patients with resectable N1 and N2 nonsmall-cell lung cancer. Ann Thorac Surg 2008;86:1092–7.
Hancock J, Rosen J, Moreno A, Kim AW, Detterbeck FC, Boffa DJ. Management of clinical stage IIIA primary lung cancers in the national cancer database. Ann Thoracic Surg. 2014;98:424-432.
De Leyn P, Lardinois D, Van Schil PE, Porta RR, Passlick B, Zielinski M, et al. ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg 2007;32:1-8.
Silvestri GA, Gonzalez AV, Jantz MA, Margolis ML, Gould MK, Tanoue LT, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143(5 Suppl):e211S-50S.
Van Klaveren RJ, Festen J, Otten HJ, Cox AL, de Graaf R, Lacquet LK. Prognosis of unsuspected but completely resectable N2 non-small cell lung cancer. Ann Thorac Surg 1993;56:300-4.
Goldstraw P, Mannam GC, Kaplan DK, Michail P. Surgical management of non-small-cell lung cancer with ipsilateral mediastinal node metastasis (N2 disease). J Thorac Cardiovasc Surg 1994;107:19-27.
De Leyn P, Schoonooghe P, Deneffe G, Van Raemdonck D, Coosemans W, Vansteenkiste J, et al. Surgery for non-small cell lung cancer with unsuspected metastasis to ipsilateral mediastinal or subcarinal nodes (N2 disease). Eur J Cardiothorac Surg 1996;10:649-54.
Cerfolio RJ, Bryant AS. Survival of patients with unsuspected N2 (stage IIIA) nonsmall-cell lung cancer. Ann Thorac Surg 2008;86:362–7.
Krantz SB, Howington JA, Wood DE, Kim KW, Kosinski AS, Cox ML , et al. Invasive mediastinal staging for lung cancer by Society of Thoracic Surgeons Database participants. Ann Thorac Surg. 2018;106:1055-62.
Little AG, Rusch VW, Bonner JA, Gaspar LE, Green MR, Webb WR, et al. Patterns of surgical care of lung cancer patients. Ann Thorac Surg. 2005;80:2051-6.
Little AG, Gay EG, Gaspar LE, Stewart AK. National survey of non-small cell lung cancer in the United States: epidemiology, pathology and patterns of care. Lung Cancer. 2007;57:253-60.
Farjah F, Flum DR, Ramsey SD, Heagerty PJ, Symons RG, Wood DE. Multi-modality mediastinal staging for lung cancer among Medicare beneficiaries. J Thorac Oncol. 2009;4:355–363.
Vest MT, Tanoue L, Soulos PR, Kim AW, Detterbeck F, Morgensztern D, et al. Thoroughness of mediastinal staging in stage IIIA non-small cell lung cancer. J Thorac Oncol. 2012;7:188-95.
Ost DE, Niu J, Elting LS, Buchholz TA, Giordano SH. Determinants of practice patterns and quality gaps in lung cancer staging and diagnosis. Chest. 2014;145:1097-113.
Ost DE, Niu J, Elting LS, Buchholz TA, Giordano SH. Quality gaps and comparative effectiveness in lung cancer staging and diagnosis. Chest. 2014;145:331-45.
Faris N, Yu X, Sareen S, Signore RS, McHugh LM, Roark K, et al. Preoperative evaluation of lung cancer in a community health care setting. Ann Thorac Surg. 2015;100:394-400.
Sawhney MS, Bakman Y, Holmstrom AM, Nelson DB, Lederle FA, Kelly RF. Impact of pre-operative endoscopic ultrasound on non-small cell lung cancer staging. Chest. 2007;132:916-21.
Bendzsak A, Waddell TK, Yasufuku K, Keshavjee S, Perrot M, Cypel M, et al. Invasive Mediastinal Staging Guideline Concordance. Ann Thorac Surg. 2017;103:1736-41.
Darling G, Dickie J, Malthaner R, Kennedy E, Tey R. Invasive mediastinal staging of non-small cell lung cancer. A Quality Initiative of the Program in Evidence-Based Care (PEBC), Cancer Care Ontario [Internet]. 2010; Evidence-Based Series 17-6. Accessed September 21, 2016.
Darling GE, Dickie AJ, Malthaner RA, Kennedy EB, Tey R. Invasive mediastinal staging of non-small-cell lung cancer: a clinical practice guideline. Curr Oncol. 2011;18:e304-10.
De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, et al. Revised ESTS guide- lines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014;45:787-98.
Call S, Obiols C, Rami-Porta R, Trujillo-Reyes JC, Iglesias M, Saumench R, et al. Video-Assisted Mediastinoscopic Lymphadenectomy for Staging Non-Small Cell Lung Cancer. Ann Thorac Surg. 2016;101:1326-33.
Riquet M, Bagan P, Barthes FL, Banu E, Scotte F, Foucault C, et al. Completely resected non-small cell lung cancer: reconsidering prognostic value and significance of N2 metastases. Ann Thorac Surg. 2007;84(6):1818-24.
Eckardt J, Jakobsen E, Licht PB. Subcarinal Lymph Nodes Should be Dissected in All Lobectomies for Non-Small Cell Lung Cancer-Regardless of Primary Tumor Location. Ann Thorac Surg. 2017;103:1121-5.
Howington JA, Blum MG, Chang AC, Balekian AA, Murthy SC. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer. 3rd ed. American College of Chest Physicians evidence- based clinical practice guidelines. Chest. 2013;143(5 Suppl): e278S-313S.
Ramnath N, Dilling TJ, Harris LJ, Kim AW, Michaud GC, Balekian AA, et al. Treatment of stage III non-small cell lung cancer: Diagnosis and management of lung cancer. 3rd ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e314S-40S.
Cerfolio RJ, Maniscalco L, Bryant AS. The treatment of patients with stage IIIA non-small cell lung cancer from N2 disease: who returns to the surgical arena and who survives. Ann Thorac Surg. 2008;86:912-20.
Wongkornrat W, Sriyoscharti S, Phanchaipetch T, Subtaweesin T, Thongchareon P, Sakiyalak P, et al. Long-Term Outcome after Pneumonectomy at Siriraj Hospital. Siriraj Med J. 2020;64(1):11-14.
Rosell R, Gomez-Codina J, Camps C, Sánchez JJ, Maestre J, Padilla J, et al. Preresectional chemotherapy in stage IIIA non-small-cell lung cancer: a 7-year assessment of a randomized controlled trial. Lung Cancer. 1999;26:7-14.
Roth J, Fossella F, Komaki R, Ryan MB, Putnam Jr JB, Lee JS, et al. A randomized trial comparing perioperative chemotherapy and surgery with surgery alone in resectable stage IIIA nonsmall- cell lung cancer. J Natl Cancer Inst. 1994;86:673-80.
Vansteenkiste JF, De Leyn PR, Deneffe GJ, Lerut TE, Demedts MG. Clinical prognostic factors in surgical treated stage IIIA-N2 non- small cell lung cancer: analysis of the literature. Lung Cancer. 1998;19:3-13.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














