Attitudes Toward Long-Acting Injectable Antipsychotics among Schizophrenia Patients in Southern Thailand: A Multihospital-Based Cross- Sectional Survey
DOI:
https://doi.org/10.33192/Smj.2022.24Keywords:
Antipsychotics, attitude, knowledge, long-acting injectable, schizophreniaAbstract
Objective: To identify the attitudes toward long-acting injectable antipsychotics (LAIs) among schizophrenia atthree psychiatric outpatient clinics in Southern Thailand from February to April 2021.
Materials and Methods: A study was conducted at three psychiatric outpatient clinics. All patients, who met the criteria of having schizophrenia based on ICD-10 criteria, aged 20-60 years were included. The questionnaires utilized were:1) Demographic information, 2) Profile of schizophrenia disorder, and 3) Attitude, knowledge, and satisfaction towards LAIs. All data were analyzed using descriptive statistics.
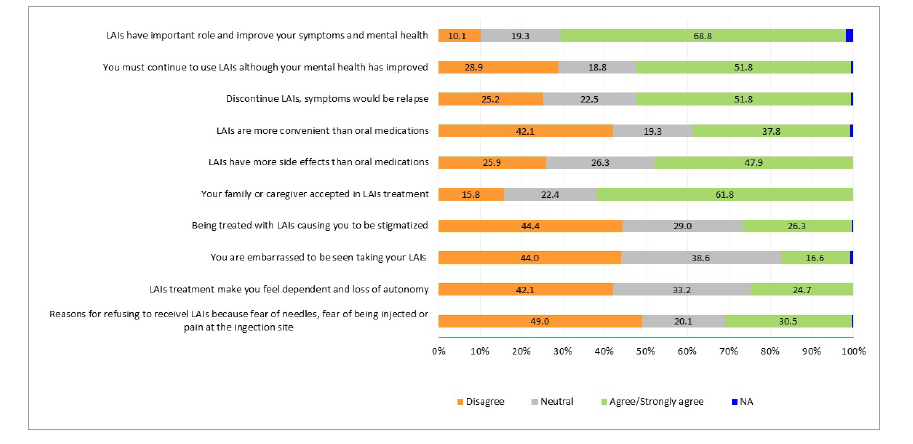
Results: There were 259 participants who completed the questionnaires. From the participants, 39% had a history of being treated with LAIs. A quarter of them felt LAIs made them feel stigmatized (26.3%), that they lost autonomy (24.7%), and embarrassed (16.6%). The reasons for refusing to receive LAIs were not fear of needles or pain at the injection site (49%), but rather that LAIs had more adverse effects than oral medications (47.9%). Half of them (51.8%) knew that they must continue to use LAIs, even though their symptoms had improved as LAIs played an important role by improving their symptoms (68.8%), and preventing relapse (51.8%). They were satisfied about having been involved in the decision making of using LAIs for their treatment (63.6%), having information on the
risk-benefits from LAIs provided to them (72.3%), and the cost of LAIs (75.2%).
Conclusion: Before deciding to prescribe LAIs, we should ensure that all patients receive information about the risks, and benefits of LAIs, boosting acceptance for this formulation and mitigating concerns about patient autonomy reduction and stigmatization.
References
Higashi K, Medic G, Littlewood KJ, Diez T, Granstrom O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3:200-18.
Poli PF, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012;69:220-29.
Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull. 1997;23:637-51.
Agrasuta T, Pitanupong J. Perceived stigma in patients with schizophrenia and caregivers in Songklanagarind Hospital: cross-sectional study. Songkla Med J. 2017;35:37-45.
Pitanupong J, Rueangwiriyanan C. Caregiver burdens in patients with schizophrenia and related factors. J Ment Health Thai. 2019;27:95-106.
Harrow M, Jobe TH. Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a
-year multifollow-up study. J Nerv Ment Dis. 2007;195(5):406-14.
Taylor M, Bonnie KY. Should long-acting (depot) antipsychotics be used in early schizophrenia? A systematic review. Aust N Z J Psychiatry. 2013;47:624-30.
Kirschner M, Theodoridou A, Fusar-Poli P, Kaiser S, Jager M. Patients’ and clinicians’ attitude towards long-acting depot antipsychotics in subjects with a first episode of psychosis. Ther Adv Psychopharmacol. 2013;3:89-99.
Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56:241-47.
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161:1-56.
Graffino M, Montemagni C, Mingrone C, Rocca P. Long acting injectable antipsychotics in the treatment of schizophrenia: a review of literature. Riv Psichiatr. 2014;49:115-23.
Heres S, Reichhart T, Hamann J, Mendel R, Leucht S, Kissling W. Psychiatrists’ attitude to antipsychotic depot treatment in patients with first-episode schizophrenia. Eur Psychiatry. 2011;26:297-301.
Aunjitsakul W, Teetharatkul T, Vitayanont A, Liabsuetrakul T. Correlations between self-reported and psychiatrist assessments of well-being among patients with schizophrenia. Gen Hosp Psychiatry. 2019;56:52-3.
Acosta FJ, Hernandez JL, Pereira J, Herrera J, Rodriguez CJ. Medication adherence in schizophrenia. World J Psychiatry. 2012;2:74-82.
Jaeger M, Rossler W. Attitudes towards long-acting depot antipsychotics: a survey of patients, relatives and psychiatrists. Psychiatry Res. 2010;175:58-62.
Geerts P, Martinez G, Schreiner A. Attitudes towards the administration of long-acting antipsychotics: a survey of physicians and nurses. BMC Psychiatry. 2013;13:58.
Walburn J, Gray R, Gournay K, Quraishi S, David AS. Systematic review of patient and nurse attitudes to depot antipsychotic medication. Br J Psychiatry. 2001;179:300-7.
Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983;13:177-83.
Rofail D, Gray R, Gournay K. The development and internal consistency of the satisfaction with Antipsychotic Medication Scale. Psychol Med. 2005;35:1063-72.
James BO, Omoaregba JO, Okonoda KM, Otefe EU, Patel MX. The knowledge and attitudes of psychiatrists towards antipsychotic long-acting injections in Nigeria. Ther Adv Psychopharmacol. 2012;2:169-77.
Ciglar M, Bjedov S, Malekovic H. Attitudes of Croatian psychiatrists towards long-acting injectable antipsychotics. Psychiatr Danub. 2016;28:273-77.
Sugawara N, Kudo S, Ishioka M, Sato Y, Kubo K, Yasui-Furukori N. Attitudes toward long-acting injectable antipsychotics among patients with schizophrenia in Japan. Neuropsychiatr Dis Treat. 2019;15:205-11.
Castle D, Morgan V, Jablensky A. Antipsychotic use in Australia: the patients’ perspective. Aust N Z J Psychiatry. 2002;36:633-41.
Patel MX, Bent-Ennakhil N, Sapin C, di Nicola S, Loze JY, Nylander AG, et al. Attitudes of European physicians towards the use of long-acting injectable antipsychotics. BMC Psychiatry. 2020;20:123.
Gray R, Spilling R, Burgess D, Newey T. Antipsychotic longacting injections in clinical practice: medication management and patient choice. Br J Psychiatry Suppl. 2009;52:S51-6.
Correll CU, Lauriello J. Using Long-Acting Injectable Antipsychotics to enhance the potential for recovery in schizophrenia. J Clin Psychiatry. 2020;81(4):MS19053AH5C.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














