The Efficacy of Inside-Out Transversus Abdominis Plane Block vs Local Infiltration before Wound Closure in Pain Management after Kidney Transplantation: A Double-blind, Randomized Trial
DOI:
https://doi.org/10.33192/Smj.2022.29Keywords:
Transversus abdominis plane block, kidney transplantation, pain management, postoperative painAbstract
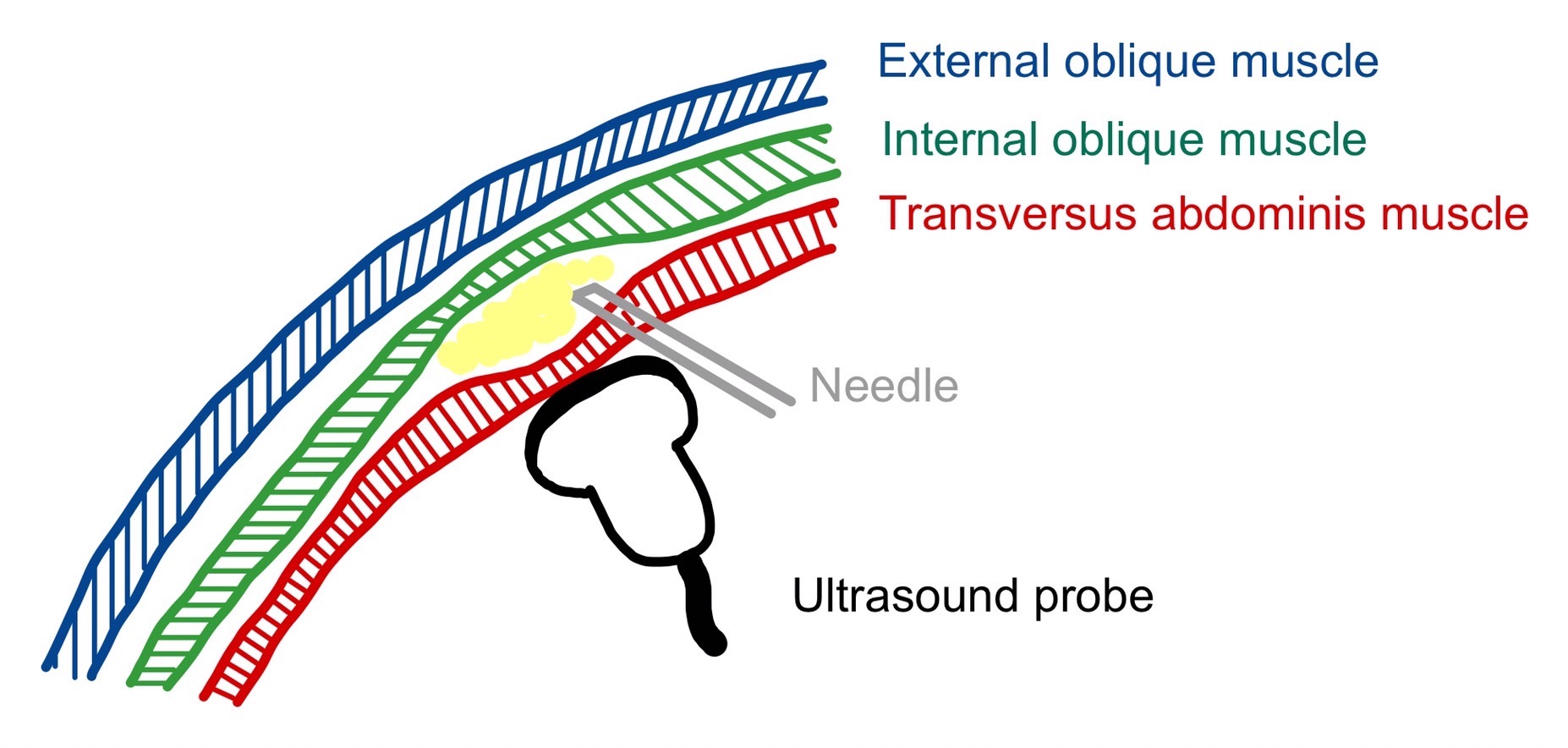
Objective: Transversus abdominis plane (TAP) block is a form of multimodal pain management in open abdominal surgery. Among patients who undergo kidney transplantation, their choice of painkillers is limited. This study aims to determine the efficacy of TAP block vs local infiltration in pain management after kidney transplantation.
Materials and Methods: In this prospective, randomized, double-blinded clinical trial, 46 patients with end-stage kidney disease who had undergone kidney transplantation were randomly divided into two groups: a local anesthetic infiltration (LA) group receiving 0.25% Bupivacaine 20 ml around the surgical wound before wound closure and a TAP block group receiving 0.25% Bupivacaine 20 ml by the inside-out technique. Their postoperative pain scores and morphine consumption were recorded at 2, 6, 12, 18, 24, and 48 hours.
Results: There was no statistically significant difference in the baseline characteristics between the groups. The postoperative pain score at two hours in the TAP block group was significantly lower than in the LA group (P value = 0.037), but without other differences in their pain scores after two hours. There was no statistical difference in the morphine consumption between the two groups. The total morphine consumption in the TAP block group was less than in the LA group, but this was not statistically significant. No patients suffered from complications of the TAP block.
Conclusion: Transversus abdominis plane block can reduce postoperative pain at two hours after kidney transplantation, without significant complications.
References
Baker M, Perazella MA. NSAIDs in CKD: Are They Safe? Am J Kidney Dis. 2020; 76(4):546-57.
Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024-26.
Tsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, et al. Transversus Abdominis Plane Block: An Updated Review 238 Volume 74, No.4: 2022 Siriraj Medical Journal https://he02.tci-thaijo.org/index.php/sirirajmedj/index of Anatomy and Techniques. Biomed Res Int. 2017;2017:8284363.
Hopkin PM. Ultrasound guidance as a gold standard in regional anaesthesia. Br J Anaesth. 2007;98(3):299-301.
Shin HJ, Kim ST, Yim KH, Lee HS, Sim JH, Shin YD. Preemptive analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing gynecologic surgery via a transverse lower abdominal skin incision. Korean J Anesthesiol. 2011;61(5):413-8.
Gharaei H, Imani F, Almasi F, Solimani M. The Effect of Ultrasound-guided TAPB on Pain Management after Total Abdominal Hysterectomy. Korean J Pain. 2013;26(4):374-8.
Chang H, Rimel BJ, Li AJ, Cass I, Karlan BY, Walsh C. Ultrasound guided transversus abdominis plane (TAP) block utilization in multimodal pain management after open gynecologic surgery. Gynecol Oncol Rep. 2018;26:75-77.
Brady RR, Ventham NT, Roberts DM, Graham C, Daniel T. Open transversus abdominis plane block and analgesic requirements
in patients following right hemicolectomy. Ann R Coll Surg Engl. 2012;94(5):327-30.
Srivastava U, Verma S, Singh TK, Gupta A, Saxsena A, Jagar KD, et al. Efficacy of trans abdominis plane block for post cesarean delivery analgesia: A double-blind, randomized trial. Saudi J Anaesth. 2015;9(3):298-302.
Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107(6):2056-60.
Azawi NH, Mosholt KS, Fode M. Unilateral ultrasound-guided transversus abdominis plane block after nephrectomy; postoperative pain and use of opioids. Nephrourol Mon. 2016;8(2):e35356.
Singh PM, Borle A, Makkar JK, Trisha A, Sinha A. Evaluation of transversus abdominis plane block for renal transplant recipients - A meta-analysis and trial sequential analysis of published studies. Saudi J Anaesth. 2018;12(2):261-71.
Sanansilp V. Pain Control System in Siriraj Hospital Postanesthesia Care Unit (PACU). Siriraj Med J. 2014;66(4):82-90.
Basta M, Sloan P. Epidural hematoma following epidural catheter placement in a patient with chronic renal failure. Can J Anaesth. 1999;46:271-4.
Sun N, Wang S, Ma P, Liu S, Shao A, Xiong L. Postoperative Analgesia by a Transversus Abdominis Plane Block Using Different Concentrations of Ropivacaine for Abdominal Surgery: A Meta-Analysis. Clin J Pain. 2017;33(9):853-63.
Collins JB, Song J, Mahabir RC. Onset and duration of intradermal mixtures of bupivacaine and lidocaine with epinephrine. Can J Plast Surg. 2013;21(1):51-53.
Yang P, Luo Y, Lin L, Zhang H, Liu Y, Li Y. The efficacy of transversus abdominis plane block with or without dexmedetomidine for postoperative analgesia in renal transplantation. A randomized controlled trial. Int J Surg. 2020;79:196-201.
Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014;112(3):427-39.
Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med. 2008;33(3):274-5.
Lancaster P, Chadwick M. Liver trauma secondary to ultrasoundguided transversus abdominis plane block. Br J Anaesth. 2010;104(4):509-10.
Narasimhulu DM, Scharfman L, Minkoff H, George B, Homel P, Tyagaraj K. A randomized trial comparing surgeonadministered intraoperative transversus abdominis plane block with anesthesiologist-administered transcutaneous block. Int J Obstet Anesth. 2018;35:26-32.
Dahl JB, Møiniche S. Pre-emptive analgesia. Br Med Bull. 2004;71:13-27.
Kolacz M, Mieszkowski M, Janiak M, Zagorski K, Byszewska B, Weryk-Dysko M, et al. Transversus abdominis plane block versus quadratus lumborum block type 2 for analgesia in renal transplantation: A randomised trial. Eur J Anaesthesiol. 2020;37(9):773-89.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














