Validation of Several Formulas to Differentiate Thalassemia from Iron Deficiency Anemia and Proposal of a Thalassemia–Iron Deficiency Discrimination (TID) Predictive Score
DOI:
https://doi.org/10.33192/Smj.2022.32Keywords:
Iron deficiency anemia, microcytic anemia, predictive score, thalassemiaAbstract
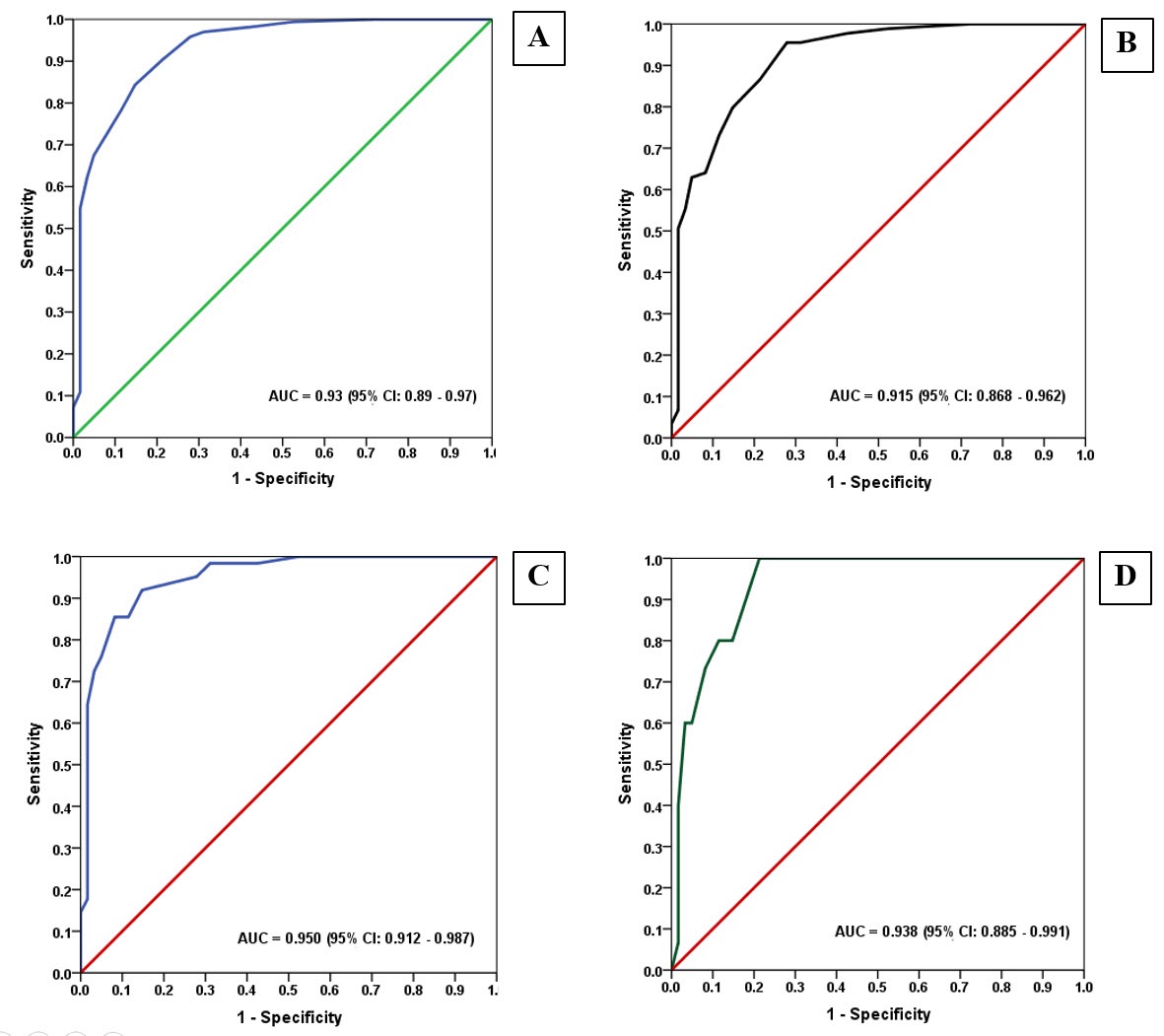
Objective: This study aimed to validate the sensitivity analysis of all the available formulas for their ability to differentiate between IDA and thalassemia and propose a novel formula to improve the sensitivity of all thalassemia subtypes screening.
Material and Methods: We conducted a 5-year, single-center, Cohort study on 227 microcytic anemia patients diagnosed between June 2015 and September 2020 at Chaophraya Yommarat Hospital, Suphanburi, Thailand to validate the sensitivity of all the available formulas and invent the novel predictive score.
Results: Approximately three-quarters of our cases were all subtypes of thalassemia diseases while 26.9% were IDA. The sensitivity of almost all the previous formulas for thalassemia prediction ranged between 13.9%-44.0%, while the specificity varied between 0%–98.4%. Nevertheless, the sensitivity of the formulas that had favorable sensitivity was quite low. Here, a novel thalassemia–iron deficiency discrimination (TID) predictive score is proposed, which demonstrated a sensitivity of 90.4% the specificity of 78.7%, the positive predictive value of 92.0 %, the negative predictive value of 75.0%, and the accuracy of 87.2%.
Conclusion: The proposed TID predictive score is a novel uncomplicated formulation which offers high sensitivity for all thalassemia subtypes prediction.
References
WHO. Trends in anemia in women and children: 1995 to 2016; WHO 2017; Available from http://www.WHO.int/data/gho/data/indicators/indicator-details/GHO/prevalence-ofanemia-in-women-of-reprodutive-age.
Brimson S, Suwanwong Y, Brimson JM. Nutritional anemia predominant form of anemia in educated young Thai women. Ethn Health. 2019;24(4):405-14. doi:10.1080/13557858.2017.1346188
Taher AT, Saliba AN. Iron overload in thalassemia: different organs at different rates. Hematology Am Soc Hematol Educ Program. 2017;2017(1):265-71. doi:10.1182/asheducation-2017.1.265
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832-43. doi:10.1056/NEJMra1401038
Brancaleoni V, Di Pierro E, Motta I, Cappellini MD. Laboratory diagnosis of thalassemia. Int J Lab Hematol. 2016;38 Suppl 1:32-40. doi:10.1111/ijlh.12527
Jayabose S, Giavanelli J, Levendoglu O, Sandoval C, Ozkayak F, Visintainer P. Differentiating iron deficiency anemia from thalassemia minor by using an RDW-based index. J Pediatr Hematol Oncol. 1999;21:314.
Green R, King R. A new red cell discriminant incorporating volume dispersion for differentiating iron deficiency anemia from thalassemia minor. Blood Cells. 1989;15(3):481-95.
Srivastava PC, Bevington JM. Iron deficiency and-or thalassaemia trait. Lancet. 1973;1(7807):832. doi:10.1016/s0140-6736(73)90637-5
Mentzer WC Jr. Differentiation of iron deficiency from thalassaemia trait. Lancet. 1973;1(7808):882. doi:10.1016/s0140-6736(73)91446-3
Ehsani M, Darvish A, Eslani A, Seighali F. A new formula for differentiation of iron deficiency anemia (IDA) and thalassemia trait (TT). Turk J Hematol 2005;22(Suppl): 268.
Ricerca BM, Storti S, d’Onofrio G, Mancini S, Vittori M, Campisi S, et al. Differentiation of iron deficiency from thalassaemia trait: a new approach. Haematologica. 1987;72(5):409-13.
England JM, Bain BJ, Fraser PM. Differentiation of iron deficiency from thalassemia trait by routine blood‐count. Lancet. 1973;1:449-52.
Sirdah M, Tarazi I, Al Najjar E, Al Haddad R. Evaluation of the diagnostic reliability of different RBC indices and formulas in the differentiation of the β‐thalassemia minor from iron deficiency in Palestinian population. Int J Lab Hematol 2007;30:324-30.
Shine I, Lal S. A strategy to detect beta‐thalassemia minor. Lancet 1977;1:692-4.
Janel A, Roszyk L, Rapatel C, Mareynat G, Berger MG, Francois A, et al. Proposal of a score combining red blood cell indices for early differentiation of beta-thalassemia minor from iron deficiency anemia. Hematology. 2011;16(2):123-7. doi:10.1179/102453311X12940641877849.
Chandra H, Shrivastava V, Chandra S, Rawat A, Nautiyal R. Evaluation of Platelet and Red Blood Cell Parameters with Proposal of Modified Score as Discriminating Guide for Iron Deficiency Anemia and β-Thalassemia Minor. J Clin Diagn Res. 2016;10(5):EC31-EC34. doi:10.7860/JCDR/2016/17672.7843
Plengsuree S, Punyamung M, Yanola J, Nanta S, Paiping K, Maneewong K, et al. Red Cell Indices and Formulas Used in Differentiation of β-Thalassemia Trait from Iron Deficiency in Thai Adults. Hemoglobin. 2015;39(4):235-9. doi:10.3109/03630269.2015.1048352
Pornprasert S, Thongsat C, Panyachadporn U. Evaluation of Applying a Combination of Red Cell Indexes and Formulas to Differentiate β-Thalassemia Trait from Iron Deficiency Anemia in the Thai Population. Hemoglobin. 2017;41(2):116-9. doi:10.1080/03630269.2017.1323763
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva, World Health Organization, 2011 (WHO/NMH/NHD/MNM/11.1). Available from: http://www.who.int/vmnis/indicators/haemoglobin. pdf, accessed[date].
Goh LPW, Chong ETJ, Lee PC. Prevalence of Alpha (α)-Thalassemia in Southeast Asia (2010-2020): A Meta-Analysis Involving 83,674 Subjects. Int J Environ Res Public Health. 2020;17(20):7354. doi:10.3390/ijerph17207354
Kattamis A, Forni GL, Aydinok Y, Viprakasit V. Changing patterns in the epidemiology of β-thalassemia. Eur J Haematol. 2020;105(6):692-703. doi:10.1111/ejh.13512
Urrechaga E, Hoffmann JJML. Critical appraisal of discriminant formulas for distinguishing thalassemia from iron deficiency in patients with microcytic anemia. Clin Chem Lab Med. 2017;55(10):1582-91. doi:10.1515/cclm-2016-0856
Hoffmann JJML, Urrechaga E. Role of RDW in mathematical formulas aiding the differential diagnosis of microcytic anemia. Scand J Clin Lab Invest. 2020;80(6):464-9. doi:10.1080/00365513.2020.1774800
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














