Implementation of Viscoelastic Hemostatic Assay-guided Therapy to Evaluate and Manage Trauma-related Bleeding: A Pilot Study from a Level 1 Trauma Center in Bangkok, Thailand
DOI:
https://doi.org/10.33192/Smj.2022.36Keywords:
Implementation, viscoelastic hemostatic assay-guided therapy, trauma-related bleeding, rotational thromboelastometry, trauma-induced coagulopathyAbstract
Objective: To evaluate the effectiveness of viscoelastic hemostatic assay (VHA)-guided therapy for assessing and managing trauma-related bleeding using a multidisciplinary team approach at a level 1 trauma center.
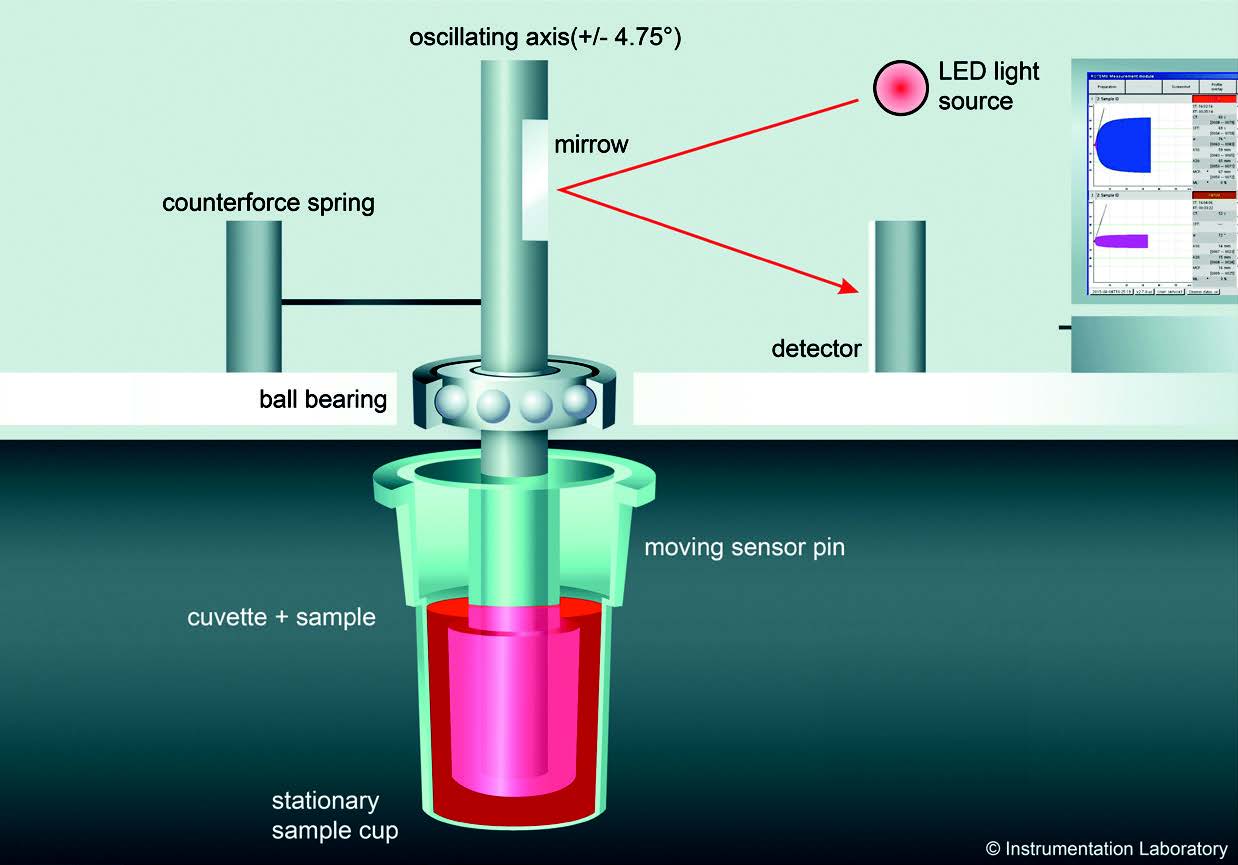
Materials and Methods: This retrospective pilot study included trauma-related hemorrhagic patients who underwent rotational thromboelastometry (ROTEM) during September 2019-May 2020. ROTEM trace results were compared with those of conventional coagulation tests (CCT).
Results: Thirteen patients (median age: 29.1 years; male: 76.92%) were included. The median (range) days of ventilator support, ICU length of stay, and hospital length of stay was 4 [0-65], 5 [1-65], and 6 [1-83], respectively. ROTEM-guided therapy was applied 26 times, and was repeated in 7 cases. Of those, four cases were repeated to correct coagulopathy. The median time-to-confirmed hemostasis for ROTEM was substantially shorter than for CCT (92 minutes [70-110] vs. 287 minutes [204-354], respectively). The coagulation results from 26 ROTEM tests were also compared between those requiring and not requiring a massive transfusion protocol (MTP). MTP with ROTEM-guided therapy was activated in 6/13 cases. Following the resuscitation endpoints in traumatic shock, four of those had their median serum lactate levels decreased from 10.9 d/L (2.1-16.8) to 3.9 d/L (1.7-17.7). ROTEM traces detected cases with low fibrinogen that only required cryoprecipitate transfusion, and red blood cell and fresh frozen plasma use was less in ROTEM than in conventional MTP.
Conclusion: VHA-guided therapy was shown to effectively facilitate goal-directed hemostatic resuscitation and efficient blood product use during resuscitation, definitive treatment, and postoperative intensive care.
References
Eastridge B, Holcomb J, Shackelford S. Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury. Transfusion. 2019;59(S2):1423-8.
Mizobata Y. Damage control resuscitation: a practical approach for severely hemorrhagic patients and its effects on trauma surgery. J Intensive Care. 2017;5(1):4.
Bugaev N, Como JJ, Golani G, Freeman JJ, Sawhney JS, Vatsaas CJ, et al. Thromboelastography and rotational thromboelastometry in bleeding patients with coagulopathy: Practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2020;89(6):999-1017.
Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. J Trauma. 2003; 54:1127–30.
Spahn D, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt B, et al. The European guideline on management of major bleeding and coagulopathy following trauma: 5th edition. Crit Care. 2019;23(1):98.
Moore EE, Moore BH, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, et al. Trauma-induced coagulopathy. Nat Rev Dis Primers. 2021.29;7(1):30.
Inaba K, Rizoli S, Veigas PV, Callum J, Davenport R, Hess J, et al. Viscoelastic Testing in Trauma Consensus Panel. 2014 Consensus conference on viscoelastic test-based transfusion guidelines for early trauma resuscitation: Report of the panel. J Trauma Acute Care Surg. 2015;78(6):1220-9.
Görlinger K, Pérez-Ferrer A, Dirkmann D, Saner F, Maegele M, Calatayud ÁAP, et al. The role of evidence-based algorithms for rotational thromboelastometry-guided bleeding management. Korean J Anesthesiol. 2019;72(4):297-322.
MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003; 55:39–44.
Brill J, Cotton B, Brenner M, Duchesne J, Ferrada P, Horer T, et al. The Role of TEG and ROTEM in Damage Control Resuscitation. Shock. 2021;56(1S):52-61.
Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38(3):298-304.
Niles SE, McLaughlin DF, Perkins JG, Wade CE, Li Y, Spinella PC, Holcomb JB. Increased mortality associated with the early coagulopathy of trauma in combat casualties. J Trauma. 2008;64(6):1459-63.
Brohi K, Cohen MJ, Ganter MT, Matthay MA, Mackersie RC, Pittet JF. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Ann Surg. 2007;245(5):812-8.
Chang R, Kerby JD, Kalkwarf KJ, Van Belle G, Fox EE, Cotton BA, et al. PROPPR Study Group. Earlier time to hemostasis is associated with decreased mortality and rate of complications: Results from the Pragmatic Randomized Optimal Platelet and Plasma Ratio trial. J Trauma Acute Care Surg. 2019;87(2):342-9.
Meyer DE, Vincent LE, Fox EE, O’Keeffe T, Inaba K, Bulger E, et al. Every minute counts: Time to delivery of initial massive transfusion cooler and its impact on mortality. J Trauma Acute Care Surg. 2017;83(1):19-24.
Gonzalez E, Moore E, Moore H. Management of Trauma-Induced Coagulopathy with Thrombelastography. Critical Care Clinics. 2017;33(1):119-34.
Toulon P, Ozier Y, Ankri A, Fleron MH, Leroux G, Samama CM. Point-of-care versus central laboratory coagulation testing during haemorrhagic surgery. A multicenter study. Thromb Haemost. 2009;101(2):394-401.
Da Luz L, Nascimento B, Shankarakutty A, Rizoli S, Adhikari N. Effect of thromboelastography (TEG®) and rotational thromboelastometry (ROTEM®) on diagnosis of coagulopathy, transfusion guidance and mortality in trauma: descriptive systematic review. Crit Care. 2014;18(5):518.
Gonzalez E, Moore EE, Moore HB, Chapman MP, Chin TL, Ghasabyan A, et al. Goal-directed Hemostatic Resuscitation of Trauma-induced Coagulopathy: A Pragmatic Randomized Clinical Trial Comparing a Viscoelastic Assay to Conventional Coagulation Assays. Ann Surg. 2016;263(6):1051-9.
Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert
G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14(2):R55.
Schochl H, Nienaber U, Maegele M, Hochleitner G, Primavesi F, Steitz B, et al. Transfusion in trauma: thromboelastometryguided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy. Crit Care. 2011;15(2):R83.
Wikkelsø A, Wetterslev J, Møller A, Afshari A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database of Systematic Reviews. 2016;2016(8):CD007871.
Stein P, Kaserer A, Sprengel K, Wanner G, Seifert B, Theusinger O, et al. Change of transfusion and treatment paradigm in major trauma patients. Anaesthesia. 2017;72(11):1317-26.
Hartert H. Blutgerinnungsstudien mit der Thrombelastographie; einem neuen Untersuchungs verfahren [Blood clotting studies with Thrombus stressography; a new Investigation procedure]. Klin Wochenschr. 1948;26(37-38):577-83. [Article in German]
De Nicola P, Mazzetti GM. Evaluation of thrombelastography. Am J Clin Pathol. 1955;23(4):447-52.
Von Kaulla KN, Weiner M. Studies of coagulation and fibrinolysis by new technic of continuous recording. Blood. 1955; 10(4):362–9.
Von Kaulla KN, Swan H. Clotting deviations in man during cardiac bypass: fibrinolysis and circulating anticoagulant. J Thorac Surg. 1958;36(4):519-30.
Kaufmann CR, Dwyer KM, Crews JD, Dols SJ, Trask AL. Usefulness of thrombelastography in assessment of trauma patient coagulation. J Trauma. 1997;42(4):716-20; discussion 720-2.
Tapia N, Chang A, Norman M, Welsh F, Scott B, Wall M, et al. TEG-guided resuscitation is superior to standardized MTP resuscitation in massively transfused penetrating trauma patients. J Trauma Acute Care Surg. 2013;74(2):378-85.
Blayney A, McCullough J, Wake E, Walters K, Campbell D, Ho D, et al. Substitution of ROTEM FIBTEM A5 for A10 in trauma: an observational study building a case for more rapid analysis of coagulopathy. Eur J Trauma Emerg Surg. 2022;48(2):1077-84.
de Vries JJ, Veen CSB, Snoek CJM, Kruip MJHA, de Maat MPM. FIBTEM clot firmness parameters correlate well with the fibrinogen concentration measured by the Clauss assay in patients and healthy subjects. Scand J Clin Lab Invest. 2020;80(7):600-5.
Olde Engberink R, Kuiper G, Wetzels R, Nelemans P, Lance M, Beckers E, et al. Rapid and Correct Prediction of Thrombocytopenia and Hypofibrinogenemia With Rotational Thromboelastometry in Cardiac Surgery. J Cardiothorac Vasc Anesth. 2014;28(2):210-216.
American College of Surgeons, editor. Massive transfusion in trauma - facs.org [Internet]. Trauma Quality Programs. American College of Surgeons; 2014 [cited 2021 Oct 25]. Available from: https://www.facs.org/-/media/files/qualityprograms/trauma/tqip/transfusion_guildelines.ashx;
Curry N, Davenport R, Pavord S, Mallett S, Kitchen D, Klein A, et al. The use of viscoelastic haemostatic assays in the management of major bleeding. Br J Haematol. 2018;182(6):789-806.
American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015;122(2):241-75.
Santos AS, Oliveira AJF, Barbosa MCL, Nogueira JLDS. Viscoelastic haemostatic assays in the perioperative period of surgical procedures: Systematic review and meta-analysis. J Clin Anesth. 2020;64:109809.
Ziegler B, Bachler M, Haberfellner H, Niederwanger C, Innerhofer P, Hell T, et al. FIinTIC study group. Efficacy of prehospital administration of fibrinogen concentrate in trauma patients bleeding or presumed to bleed (FIinTIC): A multicentre, double-blind, placebo-controlled, randomised pilot study. Eur J Anaesthesiol. 2021;38(4):348-57.
Innerhofer N, Treichl B, Rugg C, Fries D, Mittermayr M, Hell T, et al. On Behalf of the RETIC Study Group. First-Line Administration of Fibrinogen Concentrate in the Bleeding Trauma Patient: Searching for Effective Dosages and Optimal Post-Treatment Levels Limiting Massive Transfusion - Further Results of the RETIC Study. J Clin Med. 2021;10(17):3930.
CRASH-2 trial collaborators, Shakur H, Roberts I, Bautista R, Caballero J, Coats T, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23-32.
Wang IJ, Park SW, Bae BK, Lee SH, Choi HJ, Park SJ, et al. FIBTEM Improves the Sensitivity of Hyperfibrinolysis Detection in Severe Trauma Patients: A Retrospective Study Using Thromboelastometry. Sci Rep. 2020;10(1):6980.
Simmon JW, Pittet JF, Pierce B. Trauma-induced coagulopathy. Curr Anesthesiol Rep. 2014;4(3):189–99.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














