Accumulation of Advanced Glycation End Products Independently Increases the Risk of Hospitalization Among Hemodialysis Patients
DOI:
https://doi.org/10.33192/Smj.2022.37Keywords:
Hospitalization, skin autofluorescence, advanced glycation end-products, end-stage kidney diseaseAbstract
Objective: To determine the association between AGE accumulation detected by skin-autofluorescence (SAF) and hospitalization among ESKD patients.
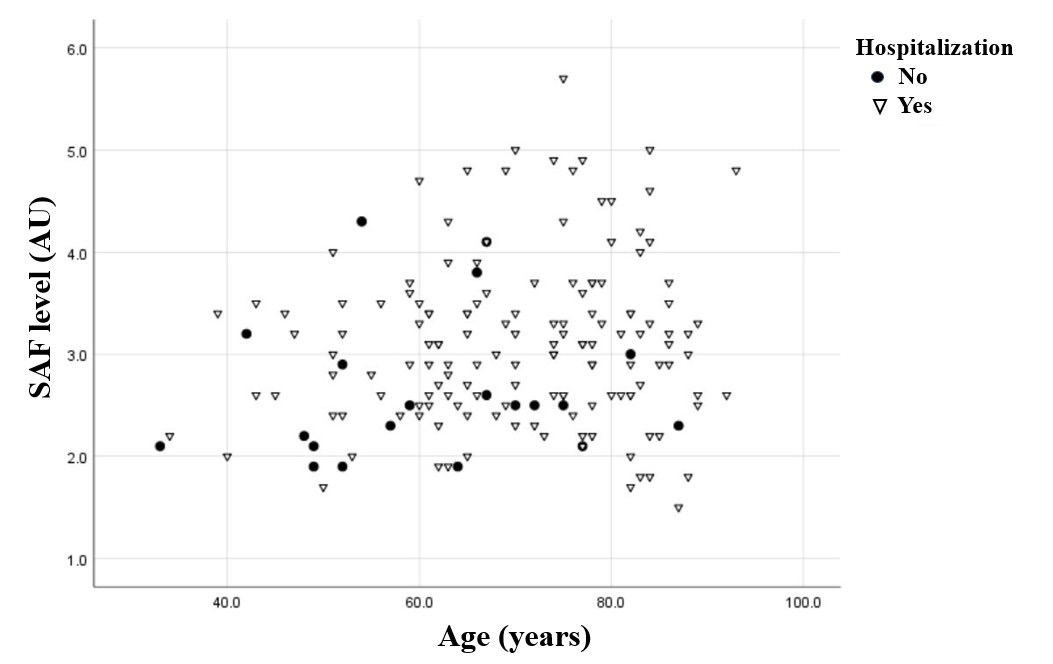
Materials and Methods: 196 ESKD patients from two hemodialysis (HD) units in Bangkok were enrolled in this retrospective study from November 2015 to March 2016. Before HD treatment, AGEs were measured with the SAF device on the area with intact skin on the volar surface of the non-fistula arm. The study concluded in December 2020, and the number of and causes of hospitalization were reviewed. A logistic regression model was used to determine the association between SAF level and patient hospitalization.
Results: Of the 196 patients enrolled in the study, SAF was measured in 165 patients with a mean (SD) age of 69.2 (13.0) years. Most of the participants were non-smokers who had hypertension and diabetes and were on high-flux dialyzers. The average weekly spKt/V was 2.1, and the mean (SD) SAF was 3.05 (0.81) AU. The group with high SAF consisted of older patients and had a higher proportion of diabetics and smokers, but this was not statistically significant when compared to the low SAF group. In the multivariable analysis model, SAF greater or equal to 3.05 AU (OR = 2.28; 95% CI, 1.05–4.94; P < 0.05) and increased age (OR = 1.05; 95% CI, 1.01–1.09; P < 0.05) were associated with an increased risk of hospitalization.
Conclusion: Higher values of age and SAF were independently associated with increased risk of hospitalization among ESKD patients.
References
Lv J-C, Zhang L-X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv Exp Med Biol. 2019;1165:3-15.
Thaweethamcharoen T, Sakulbumrungsil R, Vasuvattakul S, Nopmaneejumruslers C. Quality of life and hemoglobin levels of hemodialysis patient at Siriraj Hospital. Siriraj Med J. 2011;63:12-16.
Thaweethamcharoen T, Vasuvattakul S, Noparatayaporn P. PUK22 Comparison of Utility Score and Quality of Life Score in Thai Patient Between Twice and Thrice-Weekly Hemodialysis. Siriraj Med J. 2012;64: 94-97.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global Prevalence of Chronic Kidney Disease – A Systematic Review and Meta-Analysis. PLoS One. 2016;11(7):e0158765.
Mathew AT, Strippoli GF, Ruospo M, Fishbane S. Reducing Hospital Readmissions in Patients with End-stage Kidney Disease. Kidney Int. 2015;88(6):1250-60.
Vareesangthip K. Effect of Ultrafiltration Rate in Long Interdialytic Interval Hemodialysis Session versus Average Weekly Ultrafiltration Rate on Mortality Rate and Adverse Cardiovascular Outcomes in Maintenance Hemodialysis Patients. Siriraj Med J. 2020;72: 391-8.
Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in Chronic Kidney Disease. Pathophysiological Insights and Therapeutic Options. Circulation. 2021;143(11):1157-72.
Lacson E Jr, Bruce L, Li NC, Mooney A, Maddux FW. Depressive Affect and Hospitalization Risk in Incident Hemodialysis Patients. Clin J Am Soc Nephrol. 2014;9(10):1713-9.
Sorthananusa A, Sitawarin J, Warasompati P, Seetee T, Chirawong P. Assessment of Nutritional Status in Chronic Hemodialysis Patients at the Galayanivadhana Hemodialysis Unit. Siriraj Hosp Gaz. 2005; 57:19-36.
Kundhal K LC. Clinical Epidemiology of Cardiovascular Disease in Chronic Kidney Disease. Nephron Clin Pract. 2005;101(2):c47-52.
Peppa M, Raptis SA. Advanced Glycation End Products and Cardiovascular Disease. Curr Diabetes Rev. 2008;4(2):92-100.
Kalousová M, Sulková S, Zima T, Deppisch R, Beck W, Bednarova V, et al.Advanced Glycation End Products in Hemodialyzed Patients with Diabetes Mellitus Correlate with Leptin and Leptin/Body Fat Ratio. Ren Fail. 2003;25(2):277-86.
Thornalley PJ. Advanced Glycation End Products in Renal Failure. J Ren Nutr. 2006;16(3):178-84.
Thornalley P, Rabbani N. Highlights and Hotspots of Protein Glycation in End-Stage Renal Disease. Semin Dial. 2009;22:400-4.
Henle T, Deppisch R, Beck W, Hergesell O, Hänsch GM, Ritz E. Advanced Glycated End-products (AGE) During Haemodialysis Treatment: Discrepant Results with Different Methodologies Reflecting the Heterogeneity of AGE Compounds. Nephrol Dial Transplant. 1999;14(8):1968-75.
Nongnuch A, Davenport A. The Effect of On‐Line Hemodiafiltration, Vegetarian Diet, and Urine Volume on Advanced Glycosylation End Products Measured by Changes in Skin Auto‐Fluorescence. Artif Organs. 2018;42(11):1078-85.
Meerwaldt R, Lutgers HL, Links TP, Graaff R, Baynes JW, Gans RO, et al. Skin autofluorescence is a strong predictor of cardiac mortality in diabetes. Diabetes Care. 2007;30:107–12.
Meerwaldt R, Hartog JW, Graaff R, Huisman RJ, Links TP, Hollander NC et al. Skin Autofluorescence, A Measure of Cumulative Metabolic Stress and Advanced Glycation End Products, Predicts Mortality in Hemodialysis Patients. J Am Soc Nephrol. 2005;16(12):3687-93.
Nongnuch A, Davenport A. Skin Autofluorescence Advanced Glycosylation End Products as an Independent Predictor of Mortality in High Flux Haemodialysis and Haemodialysis Patients. Nephrology (Carlton). 2015;20(11):862-7.
Jiang J, Chen P, Chen J, Yu X, Xie D, Mei C, et al. Accumulation of Tissue Advanced Glycation End Products Correlated with Glucose Exposure Dose and Associated with Cardiovascular Morbidity in Patients on Peritoneal Dialysis. Atherosclerosis. 2012;224(1):187-94.
McIntyre NJ, Chesterton LJ, John SG, Jefferies HJ, Burton JO, Taal MW, et al. Tissue-advanced Glycation End Product Concentration in Dialysis Patients. Clin J Am Soc Nephrol. 2010;5(1):51-55.
Yue X, Hu H, Koetsier M, Graaff R, Han C. Reference Values for the Chinese Population of Skin Autofluorescence as a Marker of Advanced Glycation End Products Accumulated in Tissue. Diabet Med. 2011;28(7):818-23.
Furuya F, Shimura H, Takahashi K, Akiyama D, Motosugi A, Ikegishi Y, et al. Skin Autofluorescence is a Predictor of Cardiovascular Disease in Chronic Kidney Disease Patients. Ther Apher Dial. 2015;19(1):40-44.
Tanaka K, Tani Y, Asai J, Nemoto F, Kusano Y, Suzuki H, et al. Skin Autofluorescence is Associated with Renal Function and Cardiovascular Diseases in Pre-Dialysis Chronic Kidney Disease Patients. Nephrol Dial Transplant. 2011;26(1):214-20.
Stinghen AE, Massy ZA, Vlassara H, Striker GE, Boullier A. Uremic Toxicity of Advanced Glycation End Products in CKD. J Am Soc Nephrol. 2016;27(2):354-70.
Juliana C, Fernandes-Alnemri T, Wu J, Datta P, Solorzano L, Yu J-W, et al. Anti-inflammatory Compounds Parthenolide and Bay 11-7082 are Direct Inhibitors of the Inflammasome. J Biol Chem. 2010;285(13):9792-802.
Birukov A, Cuadrat R, Polemiti E, Eichelmann F, Schulze MB. Advanced glycation end-products, measured as skin autofluorescence, associate with vascular stiffness in diabetic, pre-diabetic and normoglycemic individuals: a cross-sectional study. Cardiovasc Diabetol. 2021;20(1):110.
Shardlow A, McIntyre NJ, Kolhe NV, Nellums LB, Fluck RJ, McIntyre CW, et al. The Association of Skin Autofluorescence with Cardiovascular Events and All-cause Mortality in Persons with Chronic Kidney Disease Stage 3: A Prospective Cohort Study. PLoS Med. 2020;17(7):e1003163.
Graaff R, Arsov S, Ramsauer B, Koetsier M, Sundvall N, Engels GE, et al. Skin and plasma autofluorescence during hemodialysis: a pilot study. Artif Organs. 2014;38(6):515-8.
Gerdemann A, Lemke HD, Nothdurft A, Heidland A, Munch G, Bahner U, et al. Low-molecular but not high-molecular advanced glycation end products (AGEs) are removed by high-flux dialysis. Clin Nephrol. 2000;54(4):276-83.
Deluyker D, Evens L, Bito V. Advanced glycation end products (AGEs) and cardiovascular dysfunction: focus on high molecular weight AGEs. Amino Acids. 2017;49(9):1535-41.
Srisuwan, W, Charoensri S, Jantarakana K, Chanchairujira T. Increasing Dialysate Flow Rate over 500 ml/Min for Reused High-Flux Dialyzers Do Not Increase Delivered Dialysis Dose: A Prospective Randomized Cross Over Study. Siriraj Med J. 2022;74:152-60.
Nongnuch A, Davenport A. The effect of vegetarian diet on skin autofluorescence measurements in haemodialysis patients. Br J Nutr. 2015;113(7):1040-3.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














