Effect of the COVID-19 Pandemic on Compliance with Contact- and Droplet-precaution Measures in Siriraj Hospital’s Internal Medicine and Pediatrics Ward Nurses
DOI:
https://doi.org/10.33192/Smj.2022.43Keywords:
COVID-19, pandemic, contact precaution, droplet precaution, complianceAbstract
Objective: To determine the effect of the COVID-19 pandemic on personal medical discipline toward infection preventive measures.
Materials and Methods: An online questionnaire on personal preventive measure was developed. The content of the questionnaire was reviewed by content experts and tested for internal consistency reliability. Nurses in the Internal Medicine and Pediatrics wards were invited to answer the questionnaire.
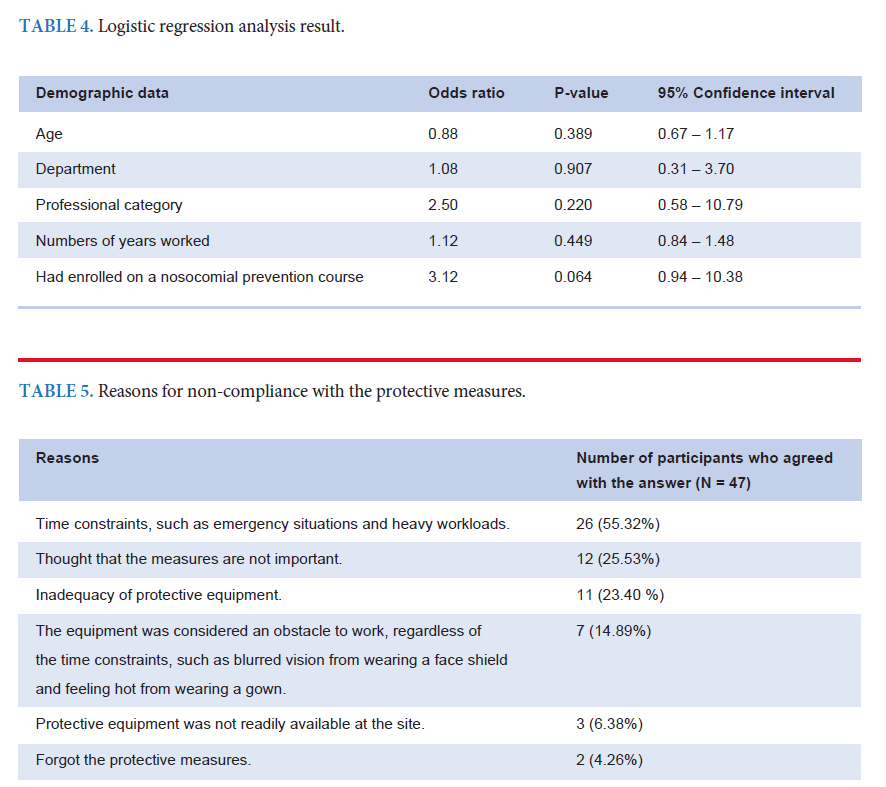
Results: In total, 188 individuals were included. Sixty-five percent of the protective measure statements showed a statistical improvement in compliance during the pandemic. Most of the protective measures, including hand washing, wearing a mask, and wearing glasses or a face shield, were statistically more complied with during the pandemic. However, some important protective measures, such as wearing a mask when performing aerosolgenerating procedures or when in close contact with droplet-precaution patients, did not show a statistically significant increase in compliance during the pandemic. There was no significant correlation between the demographic data and compliance level. The main reasons for non-compliance were time constraints, thought that the measures are not important, and equipment inadequacy.
Conclusion: During the COVID-19 pandemic, there was some improvement in compliance with contact- and dropletprecaution measures in Siriraj Hospital’s Medicine and Pediatrics wards, but compliance with measures against some high-risk procedures that can spread the infection, such as aerosol generation or contacting with droplets, were not followed properly. The importance of precaution measures should be emphasized and the adequacy of protective
equipment should be addressed to reduce the risk of spreading infection to healthcare workers and other patients.
References
Luangasanatip N, Hongsuwan M, Lubell Y, Srisamang P, Limmathurotsakul D, Cooper B. Excess length of stay due to hospital-associated infections in Thailand: 8 years retrospective data. Int J Infect Dis. 2012;16:e378-e9.
Phodha T, Riewpaiboon A, Malathum K, Coyte PC. Excess Annual Economic Burdens From Nosocomial Infections Caused by Multi-Drug Resistant Bacteria in Thailand. Expert Rev Pharmacoecon Outcomes Res. 2019;19(3):305-12.
Chokephaibulkit K, Asanathong NW, Rongrungreung Y, Assanasen S, Pumsuwan V, Wiruchkul N, et al. Epidemiology and trends of important pediatric healthcare-associated infections at Siriraj Hospital, Thailand. Southeast Asian J Trop Med Public Health. 2017;48(3):641-54.
Punpop M, Malathum P, Malathum K. Adherence of Healthcare Workers Toward the Contact Precaution Guidelines for Patients With Multidrug-Resistant Organisms in a Tertiary Care Hospital. Rama Med J. 2018;41(4):56-64.
Wasuwanich P, Thawillarp S, Ingviya T, Karnsakul W. Coronavirus Disease 2019 (COVID-19) and Its Gastrointestinal and Hepatic Manifestations. Siriraj Med J. 2020;72(4):272-8.
Swain SK, Das S, Lenka S. Sudden Sensorineural Hearing Loss among COVID-19 Patients-Our Experiences at an Indian Teaching Hospital. Siriraj Med J. 2021;73(2):77-83.
Crook H, Raza S, Nowell J, Young M, Edison P. Long covid—mechanisms, risk factors, and management. BMJ. 2021;374:n1648
Tabacof L, Tosto-Mancuso J, Wood J, Cortes M, Kontorovich A, McCarthy D, et al. Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am J Phys Med Rehabil. 2022;101:48-52.
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. 2021 [cited 2021 Jul 22]. Available from: https://covid19.who.int/
Mehta S, Machado F, Kwizera A, Papazian L, Moss M, Azoulay É, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021;9(3):226-8.
Alajmi J, Jeremijenko AM, Abraham JC, Alishaq M, Concepcion EG, Butt AA, Abou-Samra A. COVID-19 infection among healthcare workers in a national healthcare system: The Qatar experience. Int J Infect Dis. 2020;100:386-9.
Tizaoui K, Zidi I, Lee KH, Ghayda RA, Hong SH, Li H, et al. Update of the current knowledge on genetics, evolution, immunopathogenesis, and transmission for coronavirus disease 19 (COVID-19). Int J Biol Sci. 2020;16(15):2906-23.
Wong TW, Tam WW. Handwashing practice and the use of personal protective equipment among medical students after the SARS epidemic in Hong Kong. Am J Infect Control. 2005;33(10):580-6.
Jabarpour M, Dehghan M, Afsharipour G, Abaee EH, Shahrbabaki PM, Ahmadimejad M, et al. The Impact of COVID-19 Outbreak on Nosocomial Infection Rate: A Case of Iran. Can J Infect Dis Med Microbiol. 2021;2021:6650920.
Yang Q, Wang X, Zhou Q, Tan L, Zhang X and Lai X. Healthcare workers’ behavior on infection prevention and control and their determinants during the COVID-19 pandemic: a crosssectional study based on the theoretical domains framework in Wuhan, China. Arch Public Health. 2021;79(1):118.
Derek KC, Elie AA, Stephanie D, Karla S, Sally Y, Holger JS, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973-87.
Brewer NT, Cuite CL, Herrington JE, Weinstein ND. Risk compensation and vaccination: can getting vaccinated cause people to engage in risky behavior? Ann Behav Med. 2007;34(1):95-9.
Siriwittayakorn P. Announcement of the Royal College of Surgeons of Thailand on Guidance for Surgery in COVID-19 Patients. Siriraj Med J. 2020;72(5):431-5.
Kongkam P, Tiankanon K, Ratanalert S, Janthakun V, Kitiyakara T, Angsuwatcharakon P, et al. The Practice of Endoscopy during the COVID-19 Pandemic: Recommendations from the Thai Association for Gastrointestinal Endoscopy (TAGE) in collaboration with the Endoscopy Nurse Society (Thailand). Siriraj Med J. 2020;72(4):283-6.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














