Comparison of Primary Patency Rate between Drug- Coated Balloon and Plain Balloon Angioplasty in Hemodialysis Access
DOI:
https://doi.org/10.33192/Smj.2022.47Keywords:
Arteriovenous fistula (AVF), Arteriovenous graft (AVG), Paclitaxel, Drug-Coated Balloon (DCB), Plain Balloon Angioplasty (PBA), primary patency, hemodialysis accessAbstract
Objective: Hemodialysis adequacy in end-stage renal disease patients plays a crucial role in their quality of life. Repeated stenosis at the anastomotic site of arteriovenous fistula and synthetic arteriovenous graft are a major cause of access failure resulting in hospitalization, catheter usage, and contributing substantially to increased health care costs. Although standard plain balloon angioplasty (PBA) is successful, the patency rate over time is often poor. Drug-coated balloons (DCB) delivering an anti-restenosis agent, Paclitaxel, may improve patency. In this study, we aimed to investigate whether there is an increase in primary patency rate in drug-coated balloon angioplasty compared to conventional plain balloon angioplasty.
Materials and Methods: We performed a retrospective analysis of 55 patients with stenotic arteriovenous fistulas (AVF), and arteriovenous grafts (AVG) treated with DCB or PBA. Thirty-five patients were treated with drug-coated balloons, while twenty patients were treated with the standard plain balloon angioplasty. Follow up assessment was scheduled at three months, six months, and nine months. Our primary outcome was the primary patency rate, defined as the interval from the time of intervention until hemodialysis inadequacy.
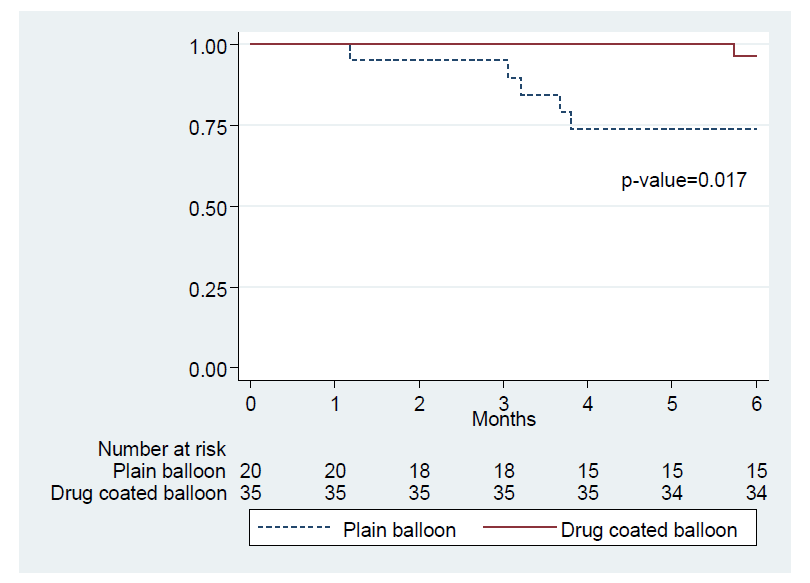
Results: There were 55 patients including twenty-one males and thirty-four females participated in the study. The average age of the 55 patients was 65.43 ± 12.89 years. Thirty (54.5%) patients were diabetes mellitus and 40 (72.7%) patients had hypertension. Seven patients (12.7%) had dyslipidemia. Eight patients (14.5%) had ischemic heart disease. And four patients (7.3%) had hyperparathyroidism. No significant differences in patency rate were found between gender, age group and patients’ underlying diseases. The proportion of primary patency rate comparing between the DCB and PBA treatment was 96.3% versus 73.9% at 6 months (P=0.017) and 92.6% versus 40% at 9 months (P<0.001). After multivariable analysis was performed (adjusted for sex, age, and underlying diseases), we found that stenosis was more likely to occur in patients who had undergone plain balloon angioplasty rather than drug-coated balloon angioplasty (HR 15.75; 95% CI 2.5%-99.1%, P=0.003).
Conclusion: Drug-coated balloon angioplasty, when compared with plain balloon angioplasty, achieves a more desirable primary patency rate at 6 months and 9 months after the procedure.
References
Kanjanabuch T, Takkavatakarn K. Global Dialysis Perspective: Thailand. Kidney 360. 2020;1:10.34067/KID.0000762020.
Annual report Thailand Renal Replacement Therapy 2020. Available from: https://www.nephrothia.org/wp-content/uploads/2021/10/Final-TRT-report-2020.pdf
Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020;75(4 Suppl 2):S1-S164.
Abdoli S, Mert M, Lee WM, Ochoa CJ, Katz SG. Network meta-analysis of drug-coated balloon angioplasty versus primary nitinol stenting for femoropopliteal atherosclerotic disease. J Vasc Surg. 2021;73(5):1802-10.
Axel DI, Kunert W, Goggelmann C, Oberhoff M, Herdeg C, Kuttner A, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997;96(2):636-45.
Lookstein RA, Haruguchi H, Ouriel K, Weinberg I, Lei L, Cihlar S, et al. Drug-Coated Balloons for Dysfunctional Dialysis Arteriovenous Fistulas. N Engl J Med. 2020;383(8):733-42.
Maya ID, Allon M. Vascular access: core curriculum 2008. Am J Kidney Dis. 2008;51(4):702-8.
Praditsuktavorn B, Wongwanit C, Chaisongrit T, Ruangsetakit C, Hongku K, Puangpanngam N. Outcomes of Autogenous Snuffbox Radiocephalic Arteriovenous Fistula-First Strategy for Hemodialysis Access. Siriraj Med J. 2019;71(6):499-505.
Diskin CJ. Novel insights into the pathobiology of the vascular access - do they translate into improved care? Blood Purif. 2010;29(2):216-29.
Lok CE, Sontrop JM, Tomlinson G, Rajan D, Cattral M, Oreopoulos G, et al. Cumulative patency of contemporary fistulas versus grafts (2000-2010). Clin J Am Soc Nephrol. 2013;8(5):810-8.
Puangpunngam N, Supokaivanich N, Ruangsetakit C, Wongwanit C, Sermsathanasawadi N, Chinsakchai K, et al. Endovascular thrombectomy versus open surgical thrombectomy for thrombosed arteriovenous hemodialysis graft. Siriraj Med J. 2019;71(6):491-8.
Roy-Chaudhury P, Sukhatme VP, Cheung AK. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006;17(4):1112-27.
Phang CC, Tan RY, Pang SC, Tan CW, The SP, Cheng RW, et al. Paclitaxel-coated balloon in the treatment of recurrent dysfunctional arteriovenous access, real-world experience and longitudinal follow up. Nephrology (Carlton). 2019;24(12):1290-5.
Yin Y, Shi Y, Cui T, Li H, Chen J, Zhang L, et al. Efficacy and Safety of Paclitaxel-Coated Balloon Angioplasty for Dysfunctional Arteriovenous Fistulas: A Multicenter Randomized Controlled Trial. Am J Kidney Dis. 2021;78(1):19-27.
Roy-Chaudhury P, Kelly BS, Miller MA, Reaves A, Armstrog J, Nanayakkara N, et al. Venous neointimal hyperplasia in polytetrafluoroethylene dialysis grafts. Kidney Int. 2001;59(6):2325-34.
Kennedy SA, Mafeld S, Baerlocher MO, Jaberi A, Rajan DK. Drug-Coated Balloon Angioplasty in Hemodialysis Circuits: A Systematic Review and Meta-Analysis. J Vasc Interv Radiol. 2019;30(4):483-94.
Trerotola SO, Lawson J, Roy-Chaudhury P, Saad TF, Lutonix AVCTI. Drug Coated Balloon Angioplasty in Failing AV Fistulas: A Randomized Controlled Trial. Clin J Am Soc Nephrol. 2018;13(8):1215-24.
Rowinsky EK, Donehower RC. Paclitaxel (taxol). N Engl J Med. 1995;332(15):1004-14.
Chen X, Liu Y, Wang J, Zhao J, Singh N, Zhang WW. A systematic review and meta-analysis of the risk of death and patency after application of paclitaxel-coated balloons in the hemodialysis access. J Vasc Surg. 2020;72(6):2186-96.
Katsanos K, Karnabatidis D, Kitrou P, Spiliopoulos S, Christeas N, Siablis D. Paclitaxel-coated balloon angioplasty vs. plain balloon dilation for the treatment of failing dialysis access: 6-month interim results from a prospective randomized controlled trial. J Endovasc Ther. 2012;19(2):263-72.
Liu C, Wolfers M, Awan BZ, Ali I, Lorenzana AM, Smith Q, et al. Drug-Coated Balloon Versus Plain Balloon Angioplasty for Hemodialysis Dysfunction: A Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2021;10(23):e022060.
Patane D, Failla G, Coniglio G, Russo G, Morale W, Seminara G, et al. Treatment of juxta-anastomotic stenoses for failing distal radiocephalic arteriovenous fistulas: Drug-coated balloons versus angioplasty. J Vasc Access. 2019;20(2):209-16.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














