The Safety of Food and Drink Consistencies Based on a Fiberoptic Endoscopic Evaluation of Swallowing Study Results in Stroke Patients with Dysphagia
DOI:
https://doi.org/10.33192/Smj.2022.48Keywords:
Diet modification, stroke, dysphagia, fiberoptic endoscopic evaluation of swallowing studyAbstract
Objective: Knowing such dysphagic stroke patients’ ability to swallow various food consistencies from instrumental investigations will help the medical staff choose the appropriate and safe food consistencies, and lead to a better swallowing outcome. This study aimed to determine the safety of food textures and drink consistencies in stroke patients with dysphagia.
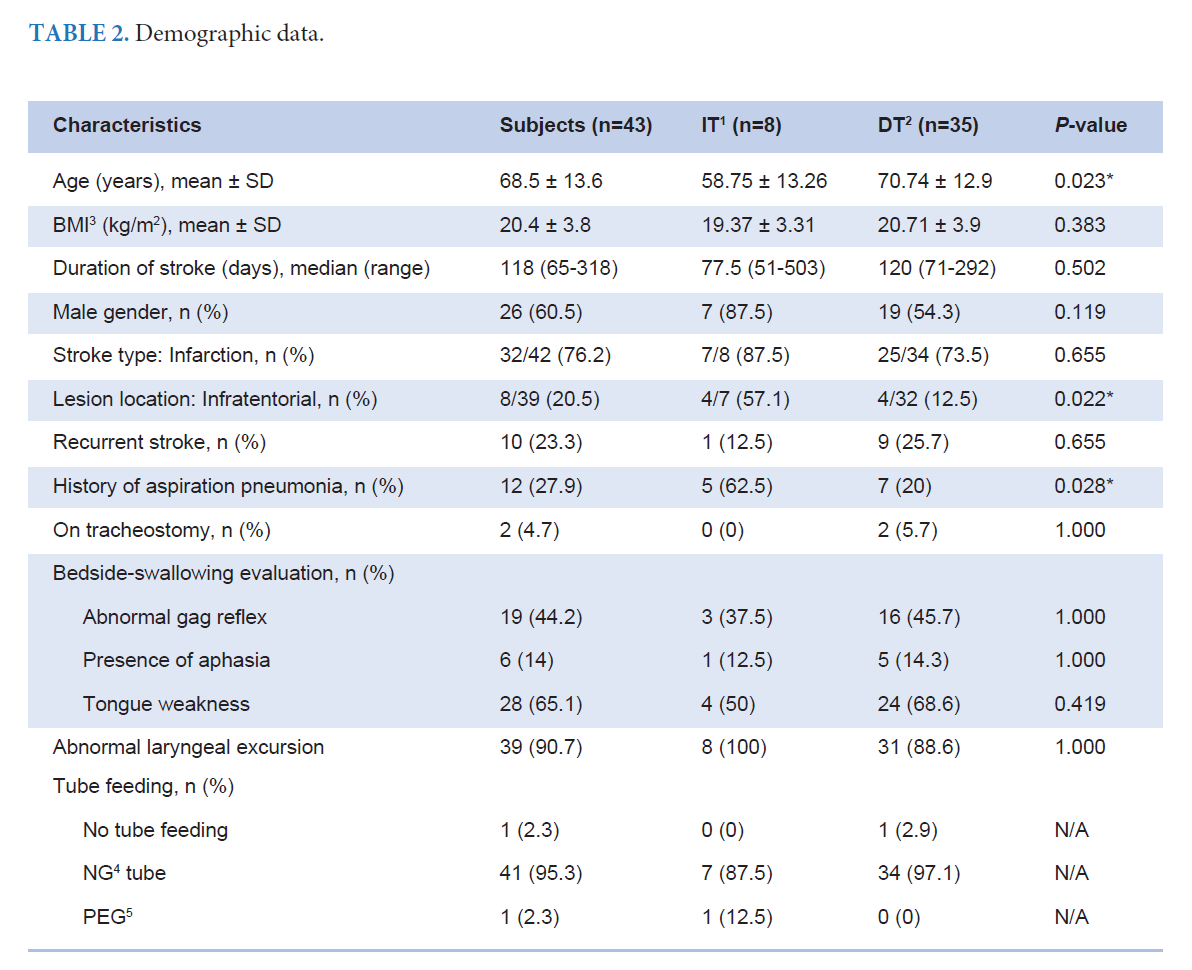
Materials and Methods: Stroke patients who failed the small-volume water swallow test (WST) and underwent fiberoptic endoscopic evaluation of swallowing (FEES) at the Department of Rehabilitation Medicine from 2017 to 2020 were reviewed. The patients’ characteristics and safe food textures and drink consistencies from their FEES results were collected. They were given a bolus test, which included four modified food textures and three varying drink consistencies, as adapted from the International Dysphagia Diet Standardization Initiative. The sequence of bolus test was adjusted by participants’ swallowing abilities individually. Moreover, their compensatory techniques were reviewed.
Results: Forty-three participants were recruited. Most of them (81.3%) could safely swallow one consistency of drink. Twenty-five (58.1%) could safely swallow a mildly thick liquid. About 20% of them could not safely swallow any food textures. Most participants (76%) who safely swallowed a mildly thick liquid could also safely swallow at least one kind of food texture. About half of them (53%) used the chin-tuck technique during the FEES testing.
Conclusion: Half of stroke patients with dysphagia who failed small-volume WST could safely swallow with a mildly thick liquid with compensatory techniques. Therefore, they should be referred to dysphagia specialists for comprehensive evaluation and management.
References
Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bull World Health Organ. 2016;94(9):634-634A.
Poungvarin N, Prayoonwiwat N, Senanarong V, Chaisevikul R, anchaivijitr C, Nilanont Y. Siriraj Acute Stroke Unit: The Experience of 614 Patients. Siriraj Med J. 2002;54(3): 151-8.
Suwanwela NC. Stroke Epidemiology in Thailand. J Stroke. 2014;16(1):1-7.
Warner JJ, Harrington RA, Sacco RL, Elkind MSV. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:3331-2.
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98-e169.
Ananchaisarp T, Sa-a K. Knowledge of stroke and planned response among patients living with diabetes mellitus and hypertension in a primary care unit. Siriraj Med J. 2022;74(2):75-84.
Ruksakulpiwat S. Intervention Enhancing Medication Adherence in Stroke Patients: An Integrative Review. Siriraj Med J. 2021;73(7):429-44.
Dajpratham P, Udompanturak S, Karawek J. Factors associated with functional improvement at discharge in stroke rehabilitation. Siriraj Med J. 2007;59:222-5.
Dajpratham P, Wechaputi C. Prevalence and Correlative Factors of Poststroke Urinary Incontinence. Siriraj Med J. 2006;58(12):1208-11.
Thanakiatpinyo T, Dajpratham P, Kovindha A, Kuptniratsaikul V. Quality of Life of Stroke Patients at 1 Year after Discharge from Inpatient Rehabilitation: A Multicenter Study. Siriraj Med J. 2021;73(4):216-23.
Martino R, Foley N, Bhopal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756-63.
Dziewas R, Michou E, Trapl-Grundschober M, Lal A, Arsava EM, Bath PM, et al. European stroke organisation and european society for swallowing disorders guideline for the diagnosis and treatment of post-stroke dysphagia. Eur Stroke J. 2021;6(3):LXXXIXCXV.
Sørensen RT, Rasmussen RS, Overgaard K, Lerche A, Johansen AM, Lindhardt T. Dysphagia screening and intensified oral hygiene reduce pneumonia after stroke. J Neurosci Nurs. 2013;45(3):139-46.
Pongakkasira C, Komaratat N, Manapunsope S, editors. Clinical practice guidelines: dysphagia. Nonthaburi: Sirindhorn National Medical Rehabilitation Institute; 2019.
Swallowing Lab, University of Toronto/University Health Network. Management of dysphagia in stroke: an educational manual for the dysphagia screening professional in the longterm care setting. Toronto: University of Toronto. University Health Network, 2016.
Brady S, Donzelli J. The modified barium swallow and the functional endoscopic evaluation of the swallowing. Otolaryngol Clin North Am. 2013;46(6):1009-22.
Rao N, Brady S, Chaudhuri G, Donzelli J, Wesling MW. Goldstandard? analysis of the videofluoroscopic and fiberoptic endoscopic swallow examinations. J Appl Res 2003; 3:89-96.
Brodsky MB, Suiter DM, Fernández MG, Michtalik HJ, Frymark TB, Venediktov E, et al. Screening accuracy for aspiration using bedside water swallow tests: A systematic review and metaanalysis. Chest. 2016;150(1):148-63.
Maeda K, Koga T, Akagi J. Tentative nil per os leads to poor outcomes in older adults with aspiration pneumonia. Clin Nutr. 2016;35(5):1147-50.
Drulia TC, Ludlow CL. Relative efficacy of swallowing versus non-swallowing tasks in dysphagia rehabilitation: current evidence and future directions. Curr Phys Med Rehabil Reports. 2013;1:242-56.
Robbins J, Butler SG, Daniels SK, Gross RD, Langmore S, Lazarus CL, et al. Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. J Speech Lang Hear Res. 2008;51(1):276-300.
Catriona M, Woroud A, Sona A. The Influence of food texture and liquid consistency modification on swallowing physiology and function: A Systematic Review. Dysphagia. 2015;30(2):272-3.
Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30(1):2-26. doi: 10.1007/s00455-014-9578-x.
Benjapornlert P, Tuakta P, Kimhiah B, Wongphaet P, Kriengsinyos W, Wattanapan P, et al. Food and Liquid Consistency Modification for Safe Swallowing in Elderly with Dysphagia Risk. Asean J Rehabil Med. 2020;30(2):60-5.
O’Keeffe ST. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified?. BMC Geriatr. 2018;18(1):167. doi: 10.1186/s12877-018-0839-7
Rosenbek JC, Robbins J, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11:93-8.
Butler SG, Markley L, Sanders B, Stuart A. Reliability of the Penetration Aspiration Scale with Flexible Endoscopic Evaluation of Swallowing. Ann Otol Rhinol Laryngol. 2015;124(6):480-3.
Cichero J, Lam P, Steele C, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: The IDDSI framework. Dysphagia. 2017;32:293-314.
Kagaya H, Inamoto Y, Okada S, Saitoh E. Body positions and functional training to reduce aspiration in patients with dysphagia. JMAJ. 2011;54(1):35-8.
Daniels SK, Pathak S, Mukhi SV, Stach CB, Morgan RO, Anderson JA, et al. The reationship between lesion localization and dysphagia in acute stroke. Dysphagia. 2017;32(6):777-84.
Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil. 2000;79:170-5.
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














