Deep Peroneal Nerve: From an Anatomical Basis to Clinical Implementation
DOI:
https://doi.org/10.33192/Smj.2022.54Keywords:
Deep peroneal nerve, accessory deep peroneal nerve, nerve imaging, nerve block, electrophysiological study, surgical reconstructionAbstract
The deep peroneal nerve (DPN) is considered one of the clinically significant nerves of the lower extremity since several clinical abnormalities can commonly be caused by its defects, either in its sensory or motor functions. Its derivatives, classified as muscular, cutaneous, and articular, mainly supply the muscles in the anterior fascial compartment of the leg and the dorsum of the foot, the 1st dorsal web space of the foot, the ankle joint, and certain joints of the foot. To improve the effectiveness of clinical practices involving the DPN, it is important to first understand its anatomical nature, including its typical characteristics and the variants (orientation, branching, and analogous structure), prior to applying such practices in clinical implementation. This review, therefore, aims to review the previously studied information of DPN on its fundamental anatomy and link it to the provided examples of current commonly used procedures, both non-invasive and invasive, e.g., nerve imaging, nerve block, neuroelectrophysiological study, and free autologous tissue transfer, thereby giving an integrated view in the translational medicine of DPN. Conclusively, the ultimate goal of this review is to help maximize the therapeutic effectiveness and to minimize the unanticipated complications of any clinical practices involving the DPN by inferring from its anatomical knowledge.
References
Standring S, editor. Gray’s anatomy: the anatomical basis of clinical practice. 41st ed. Philadelphia: Elsevier; 2016.
Demiroglu M, Ozkan K, Kilic B, Akcal A, Akkaya M, Ozkan FU. Deep peroneal nerve palsy due to osteochondroma arising from fibular head and proximal lateral tibia. Int J Surg Case Rep. 2017;31:200-2.
Itou J, Itoh M, Maruki C, Tajimi T, So T, Kuwashima U, et al. Deep peroneal nerve has a potential risk of injury during openwedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1372-9.
Lu H, Chen L, Jiang S, Shen H. A rapidly progressive foot drop caused by the posttraumatic Intraneural ganglion cyst of the deep peroneal nerve. BMC Musculoskelet Disord. 2018;19(1):298.
Lui TH. Extensor tendons and deep peroneal nerve adhesion: treated by complete anterior ankle arthroscopic capsulotomy. Foot Ankle Surg. 2012;18(1):e1-3.
Takahashi S, Ogose A, Tajino T, Osanai T, Okada K. Osteosarcoma of the proximal fibula. An analysis of 13 cases in the northern Japan. Ups J Med Sci. 2007;112(3):366-72.
Stitgen SH, Cairns ER, Ebraheim NA, Niemann JM, Jackson WT. Anatomic considerations of pin placement in the proximal tibia and its relationship to the peroneal nerve. Clin Orthop Relat Res. 1992(278):134-7.
Soejima O, Ogata K, Ishinishi T, Fukahori Y, Miyauchi R. Anatomic considerations of the peroneal nerve for division of the fibula during high tibial osteotomy. Orthop Rev. 1994;23(3):244-7.
Chompoopong S, Apinhasmit W, Sangiampong A, Amornmettajit N, Charoenwat B, Rattanathamsakul N, et al. Anatomical considerations of the deep peroneal nerve for biopsy of the proximal fibula in Thais. Clin Anat. 2009;22(2):256-60.
Takeda A, Tsuchiya H, Mori Y, Tanaka S, Kikuchi S, Tomita K. Anatomical aspects of biopsy of the proximal fibula. Int Orthop. 2001;24(6):335-7.
Ryan W, Mahony N, Delaney M, O’Brien M, Murray P. Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat. 2003;16(6):501-5.
Lawrence SJ, Botte MJ. The deep peroneal nerve in the foot and ankle: an anatomic study. Foot Ankle Int. 1995;16(11):724-8.
Ranade AV, Rajanigandha V, Rai R, Ebenezer DA. Relationship between the deep peroneal nerve and dorsalis pedis artery in the foot: a cadaveric study. Clin Anat. 2008;21(7):705-12.
Aktan Ikiz ZA, Ucerler H, Uygur M. Dimensions of the anterior tarsal tunnel and features of the deep peroneal nerve in relation to clinical application. Surg Radiol Anat. 2007;29(7):527-30.
Ikiz ZA, Ucerler H, Uygur M. The clinical importance of the relationship between the deep peroneal nerve and the dorsalis pedis artery on the dorsum of the foot. Plast Reconstr Surg. 2007;120(3):690-6.
Chitra R. The relationship between the deep fibular nerve and the dorsalis pedis artery and its surgical importance. Indian J Plast Surg. 2009;42(1):18-21.
Rab M, Ebmer J, Dellon AL. Innervation of the sinus tarsi and implications for treating anterolateral ankle pain. Ann Plast Surg. 2001;47(5):500-4.
Bryce TH. Long muscular branch of the musculocutaneous nerve of the leg. J Anat. 1896;31:5-12.
Prakash, Bhardwaj AK, Singh DK, Rajini T, Jayanthi V, Singh G. Anatomic variations of superficial peroneal nerve: clinical implications of a cadaver study. Ital J Anat Embryol. 2010;115(3):223-8.
Mathis S, Ciron J, du Boisgueheneuc F, Godeneche G, Hobeika L, Larrieu D, et al. Study of accessory deep peroneal nerve motor conduction in a population of healthy subjects. Neurophysiol Clin. 2011;41(1):29-33.
Kudoh H, Sakai T, Horiguchi M. The consistent presence of the human accessory deep peroneal nerve. J Anat. 1999;194(Pt 1):101-8.
Lambert EH. The accessory deep peroneal nerve. A common variation in innervation of extensor digitorum brevis. Neurology. 1969;19(12):1169-76.
Murad H, Neal P, Katirji B. Total innervation of the extensor digitorum brevis by the accessory deep peroneal nerve. Eur J Neurol. 1999;6(3):371-3.
Tomaszewski KA, Roy J, Vikse J, Pekala PA, Kopacz P, Henry BM. Prevalence of the accessory deep peroneal nerve: a cadaveric study and meta-analysis. Clin Neurol Neurosurg. 2016;144:105-11.
Saba EK. Electrophysiological study of accessory deep peroneal nerve in a sample of Egyptian subjects. Egypt Rhematol Rehabil. 2019;46:251-6.
Sinanovic O, Zukic S, Muftic M, Tinjic N. Prevalence of accessory deep peroneal nerve in sample of Bosnia and Herzegovina subjects: an electrophysiological study. Acta Inform Med. 2021;29(3):193-6.
Crutchfield CA, Gutmann L. Hereditary aspects of accessory deep peroneal nerve. J Neurol Neurosurg Psychiatry. 1973;36(6):989-90.
Bianchi S, Martinoli C, editors. Ultrasound of the musculoskeletal system. Berlin: Springer; 2007.
Blitz NM, Amrami KK, Spinner RJ. Magnetic resonance imaging of a deep peroneal intraneural ganglion cyst originating from the second metatarsophalangeal joint: a pattern of propagation supporting the unified articular (synovial) theory for the formation of intraneural ganglia. J Foot Ankle Surg. 2009;48(1):80-4.
Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR Am J Roentgenol. 2008;190(6):1621-6.
Yablon CM, Hammer MR, Morag Y, Brandon CJ, Fessell DP, Jacobson JA. US of the peripheral nerves of the lower extremity: a landmark approach. Radiographics. 2016;36(2):464-78.
Rumack CM, Levine D, editors. Diagnostic ultrasound. 5th ed. Philadelphia: Elsevier; 2018. 2 vol.
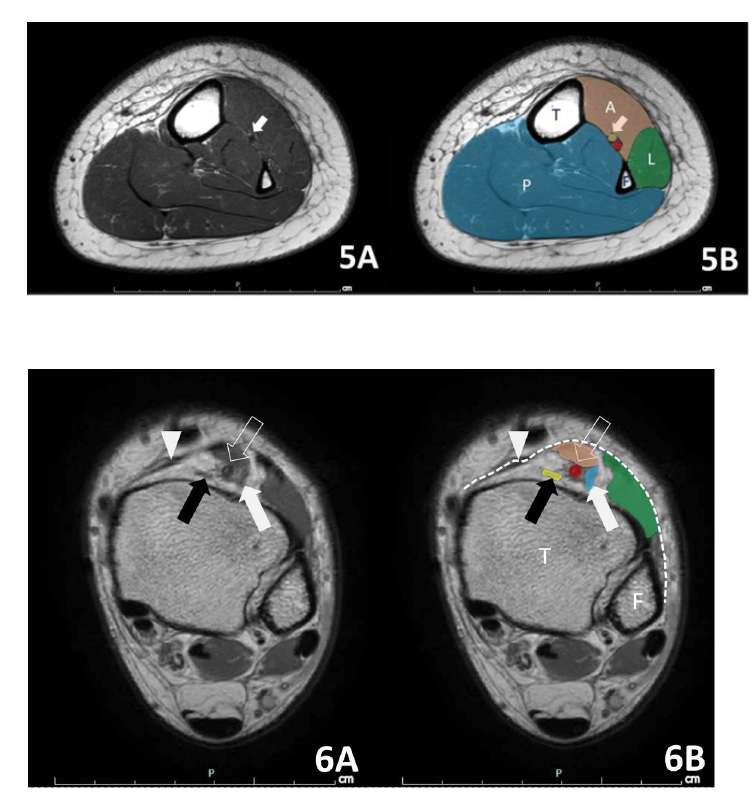
Becciolini M, Pivec C, Riegler G. Ultrasound imaging of the deep peroneal nerve. J Ultrasound Med. 2021;40(4):821-38.
Weig SG, Waite RJ, McAvoy K. MRI in unexplained mononeuropathy. Pediatr Neurol. 2000;22(4):314-7.
Panda S, Gourie-Devi M, Sharma A, Sud A. Isolated deep peroneal nerve palsy: role of magnetic resonance imaging in localization. Ann Indian Acad Neurol. 2015;18(4):451-3.
Vohra S, Arnold G, Doshi S, Marcantonio D. Normal MR imaging anatomy of the thigh and leg. Magn Reson Imaging Clin N Am. 2011;19(3):621-36.
Beggs I. Pictorial review: imaging of peripheral nerve tumours. Clin Radiol. 1997;52(1):8-17.
Ahlawat S, Belzberg AJ, Montgomery EA, Fayad LM. MRI features of peripheral traumatic neuromas. Eur Radiol. 2016;26(4):1204-12.
Hiramatsu K, Yonetani Y, Kinugasa K, Nakamura N, Yamamoto K, Yoshikawa H, et al. Deep peroneal nerve palsy with isolated lateral compartment syndrome secondary to peroneus longus tear: a report of two cases and a review of the literature. J Orthop Traumatol. 2016;17(2):181-5.
Rowdon GA, Richardson JK, Hoffmann P, Zaffer M, Barill E. Chronic anterior compartment syndrome and deep peroneal nerve function. Clin J Sport Med. 2001;11(4):229-33.
Henrot P, Stines J, Walter F, Martinet N, Paysant J, Blum A. Imaging of the painful lower limb stump. Radiographics. 2000;20 Spec No:S219-35.
Kransdorf MJ, Murphey MD. Imaging of soft tissue tumors. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2006.
Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. Radiographics. 2010;30(4):1001-19.
Neto N, Nunnes P. Spectrum of MRI features of ganglion and synovial cysts. Insights Imaging. 2016;7(2):179-86.
Bermejo A, De Bustamante TD, Martinez A, Carrera R, Zabia E, Manjon P. MR imaging in the evaluation of cystic-appearing soft-tissue masses of the extremities. Radiographics. 2013;33(3):833-55.
Sallomi D, Janzen DL, Munk PL, Connell DG, Tirman PF. Muscle denervation patterns in upper limb nerve injuries: MR imaging findings and anatomic basis. AJR Am J Roentgenol. 1998;171(3):779-84.
Galloway HR. Muscle denervation and nerve entrapment syndromes. Semin Musculoskelet Radiol. 2010;14(2):227-35.
Albayda J, van Alfen N. Diagnostic value of muscle ultrasound for myopathies and myositis. Curr Rheumatol Rep. 2020;22(11):82.
Bendszus M, Koltzenburg M, Wessig C, Solymosi L. Sequential MR imaging of denervated muscle: experimental study. AJNR Am J Neuroradiol. 2002;23(8):1427-31.
Kopka A, Serpell MG. Distal nerve blocks of the lower limb. Contin Educ Anaesth Crit Care Pain. 2005;5(5):166-70.
Pilny J, Kubes J. Operace prednozí ve svodné anestezii nohy [Forefoot surgery under regional anesthesia]. Acta Chir Orthop Traumatol Cech. 2005;72(2):122-4. Czech.
Gropper MA, Cohen NH, Eriksson LI, Fleisher LA, Leslie K, Wiener-Kronish JP, editors. Miller’s anesthesia. 9th ed. Philadelphia: Elsevier; 2020. 2 vol.
Fung G, Liu SE. Regional anaesthesia for orthopaedic procedures. Anaesth Intensive Care Med. 2021;22(1):13–8.
Karmakar MK, editor. Musculoskeletal ultrasound for regional anaesthesia and pain medicine. 2nd ed. Hong Kong: The Chinese University of Hong Kong; 2016.
Marhofer P, Schrogendorfer K, Wallner T, Koinig H, Mayer N, Kapral S. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med. 1998;23(6):584-8.
Eichenberger U, Stockli S, Marhofer P, Huber G, Willimann P, Kettner SC, et al. Minimal local anesthetic volume for peripheral nerve block: a new ultrasound-guided, nerve dimension-based method. Reg Anesth Pain Med. 2009;34(3):242-6.
Latzke D, Marhofer P, Zeitlinger M, Machata A, Neumann F, Lackner E, et al. Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth. 2010;104(2):239-44.
Antonakakis JG, Scalzo DC, Jorgenson AS, Figg KK, Ting P, Zuo Z, et al. Ultrasound does not improve the success rate of a deep peroneal nerve block at the ankle. Reg Anesth Pain Med. 2010;35(2):217-21.
Buschbacher RM. Peroneal nerve motor conduction to the extensor digitorum brevis. Am J Phys Med Rehabil. 1999;78(6 Suppl):S26-31.
Buschbacher RM. Reference values for peroneal nerve motor conduction to the tibialis anterior and for peroneal vs. tibial latencies. Am J Phys Med Rehabil. 2003;82(4):296-301.
Lo YL, Leoh TH, Dan YF, Tan YE, Nurjannah S, Fook-Chong S. An electrophysiological study of the deep peroneal sensory nerve. Eur Neurol. 2003;50(4):244-7.
Manning C, Cook S, Rand R, Mills J, Thomas A, Galloway K. Communications between the superficial and deep fibular nerves in the foot: an anatomical and electrophysiological study. Clin Anat. 2021;34(4):544-9.
Marchini C, Zambito Marsala S, Fabris F, Fornasier A, Ferracci F. Peroneal nerve orthodromic sensory conduction technique: normative data. Neurol Sci. 2009;30(3):201-5.
Dumitru D, Diaz CA, King JC. Prevalence of denervation in paraspinal and foot intrinsic musculature. Am J Phys Med Rehabil. 2001;80(7):482-90.
Logullo F, Ganino C, Lupidi F, Perozzi C, Di Bella P, Provinciali L. Anterior tarsal tunnel syndrome: a misunderstood and a misleading entrapment neuropathy. Neurol Sci. 2014;35(5):773-5.
Katirji MB, Wilbourn AJ. Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesions. Neurology. 1988;38(11):1723-8.
Karakis I, Khoshnoodi M, Liew W, Nguyen ES, Jones HR, Darras BT, et al. Electrophysiologic features of fibular neuropathy in childhood and adolescence. Muscle Nerve. 2017;55(5):693-7.
Derr JJ, Micklesen PJ, Robinson LR. Predicting recovery after fibular nerve injury: which electrodiagnostic features are most useful? Am J Phys Med Rehabil. 2009;88(7):547-53.
Bsteh G, Wanschitz JV, Gruber H, Seppi K, Loscher WN. Prognosis and prognostic factors in non-traumatic acute-onset compressive mononeuropathies - radial and peroneal mononeuropathies. Eur J Neurol. 2013;20(6):981-5.
Marciniak C, Armon C, Wilson J, Miller R. Practice parameter: utility of electrodiagnostic techniques in evaluating patients with suspected peroneal neuropathy: an evidence-based review. Muscle Nerve. 2005;31(4):520-7.
Greyson MA, Wilkens SC, Sood RF, Winograd JM, Eberlin KR, Donelan MB. Five essential principles for first web space reconstruction in the burned hand. Plast Reconstr Surg. 2020;146(5):578e-587e.
Kalliainen LK, Schubert W. The management of web space contractures. Clin Plast Surg. 2005;32(4):503-14.
Moody L, Galvez MG, Chang J. Reconstruction of first web space contractures. J Hand Surg Am. 2015;40(9):1892-5.
Dantzer E, Queruel P, Salinier L, Palmier B, Quinot JF. Dermal regeneration template for deep hand burns: clinical utility for both early grafting and reconstructive surgery. Br J Plast Surg. 2003;56(8):764-74.
Hudson DA. Some thoughts on choosing a Z-plasty: the Z made simple. Plast Reconstr Surg. 2000;106:665-71.
Dautel G, Merle M. Direct and reverse dorsal metacarpal flaps. Br J Plast Surg. 1992;45(2):123-30.
Amouzou KS, Berny N, El Harti A, Diouri M, Chlihi A, Ezzoubi M. The pedicled groin flap in resurfacing hand burn scar release and other injuries: a five-case series report and review of the literature. Ann Burns Fire Disasters. 2017;30(1):57-61.
Woo SH, Seul JH. Optimizing the correction of severe postburn hand deformities by using aggressive contracture releases and fasciocutaneous free-tissue transfers. Plast Reconstr Surg. 2001;107(1):1-8.
Muller-Seubert W, Horch RE, Schmidt VF, Ludolph I, Schmitz M, Arkudas A. Retrospective analysis of free temporoparietal fascial flap for defect reconstruction of the hand and the distal upper extremity. Arch Orthop Trauma Surg. 2021;141(1):165-71.
Woo SH, Choi BC, Oh SJ, Seul JH. Classification of the first web space free flap of the foot and its applications in reconstruction of the hand. Plast Reconstr Surg. 1999;103(2):508-17.
Zucker RM, Gur E, Hussain G, Manktelow RT. Facial paralysis. In: Rodriguez ED, Losee JE, Neligan PC, editors. Plastic surgery. 4th ed. Vol. 3, Craniofacial, head and neck surgery and pediatric plastic surgery. Philadelphia: Elsevier; 2018. p. 329-57.
Alagoz MS, Alagoz AN, Comert A. Neuroanatomy of extensor digitorum brevis muscle for reanimation of facial paralysis. J Craniofac Surg. 2011;22(6):2308-11.
Mathes SJ, Nahai F. Classification of the vascular anatomy of muscles: experimental and clinical correlation. Plast Reconstr Surg. 1981;67(2):177-87.
Pai CH, Lin GT, Lin SY, Lin SD, Lai CS. Extensor digitorum brevis rotational muscle flap for lower leg and ankle coverage. J Trauma. 2000;49(6):1012-6.
Sugg KB, Kim JC. Dynamic reconstruction of the paralyzed face, part II: Extensor digitorum brevis, serratus anterior, and anterolateral thigh. Oper Tech Otolaryngol Neck Surg. 2012; 23(4):275-81.
Rao VK, Butler JA. Microneurovascular free transfer of extensor digitorum brevis muscle for facial reanimation. In: Strauch B, Vasconez LO, Hall-Findlay EJ, editors. Grabb’s encyclopedia of flaps. Vol. 3, Torso, pelvis, and lower extremities. Boston: Little, Brown; 1990. p. 613-7.
Mayou BJ, Watson JS, Harrison DH, Parry CB. Free microvascular and microneural transfer of the extensor digitorum brevis muscle for the treatment of unilateral facial palsy. Br J Plast Surg. 1981;34(3):362-7.
Akaranuchat N. Lower extremity reconstruction with vascularized free-tissue transfer: 20 years of experience in the faculty of medicine Siriraj hospital, Mahidol university, Bangkok, Thailand. Siriraj Med J. 2021;73(7):462–70.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














