Hidden Neuropathic Pain in Chronic Low Back Pain: Prevalence, Pattern, and Impact on Quality of Life
DOI:
https://doi.org/10.33192/Smj.2022.57Keywords:
Neuropathic pain, chronic low back pain, quality of life, low back pain, ThailandAbstract
Objective: A patient with Neuropathic Pain (NP) may suffer from pure NP or may have mixed nociceptive and neuropathic pain. No previous study has investigated NP among Thai patients with Chronic Low Back Pain (CLBP). This study aimed to investigate the prevalence and clinical presentation of NP, and the impact of NP on Quality of Life (QoL) in Thai Chronic Low Back Pain (CLBP) patients.
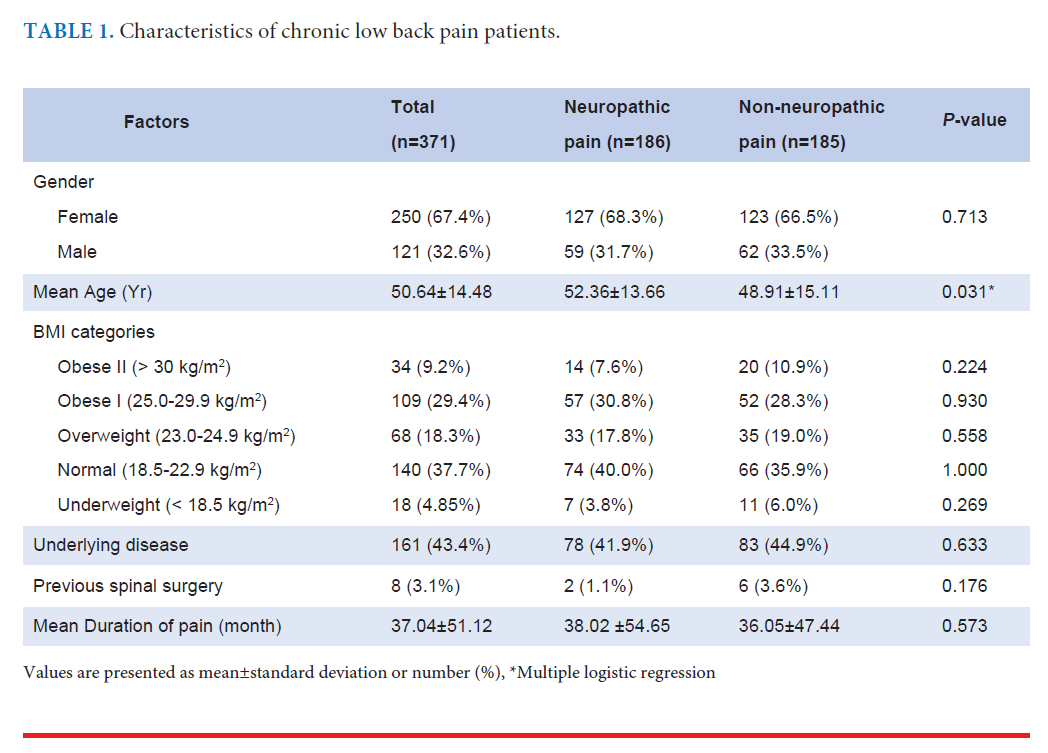
Materials and Methods: Adult patients with CLBP longer than 3 months were included. NP was detected by painDETECT questionnaire, and NP was defined as a score 19. Demographic data, pain characteristics, treatment, Oswestry Disability Index (ODI), and quality of life score (Short Form 36, SF-36) were recorded.
Results: 371 CLBP patients were enrolled. The overall prevalence of neuropathic pain was 50.1% (95% CI: 44.9-55.3%). The prevalence of NP in patients with axial low back pain, back pain with pain radiating above the knee, and back pain with pain radiating below the knee was 28.3%, 58.21%, and 59.5%, respectively. Only 48.9% of patients with NP received neuropathic pain medication. Multivariate analysis showed only older age to be associated with NP (OR: 1.017, 95% CI: 1.002-1.033). NP patients had a significantly higher ODI score. There is no difference in most dimension of SF-36 scores, except marginally higher general health and vitality dimension scores.
Conclusion: Prevalence of NP in Thai CLBP patients is high. Additionally, it is undertreated and associated with higher disability especially among patients with radiating pain above the knee. Older age is an independent predictor of NP.
References
Iizuka Y, Iizuka H, Mieda T, Tsunoda D, Sasaki T, Tajika T, et al. Prevalence of Chronic Nonspecific Low Back Pain and Its Associated Factors among Middle-Aged and Elderly People: An Analysis Based on Data from a Musculoskeletal Examination in Japan. Asian Spine J 2017;11:989-97.
Meucci RD, Fassa AG, Faria NM. Prevalence of chronic low back pain: systematic review. Rev Saude Publica 2015;49:1.
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians, Denberg TD, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 2017;166:514-30.
El Sissi W, Arnaout A, Chaarani MW, Fouad M, Assuity EI W, Zalzala M, et al. Prevalence of neuropathic pain among patients with chronic low-back pain in the Arabian Gulf Region assessed using the leeds assessment of neuropathic symptoms and signs pain scale. J Int Med Res 2010;38:2135-45.
Mehra M, Hill K, Nicholl D, Schadrack J. The burden of chronic low back pain with and without a neuropathic component: a healthcare resource use and cost analysis. J Med Econ 2012;15(2):245-52.
Gudala K, Bansal D, Vatte R, Ghai B, Schifano F, Boya C. High Prevalence of Neuropathic Pain Component in Patients with Low Back Pain: Evidence from Meta-Analysis. Pain Physician 2017;20:343-52.
Kaki AM, El-Yaski AZ, Youseif E. Identifying neuropathic pain among patients with chronic low-back pain: use of the Leeds Assessment of Neuropathic Symptoms and Signs pain scale. Reg Anesth Pain Med 2005;30:422-8.
Freynhagen R, Baron R. The evaluation of neuropathic components in low back pain. Curr Pain Headache Rep 2009;13:185-90.
Kim JH, Hong JT, Lee CS, Kim KS, Suk KS, Kim JH, et al. Prevalence of Neuropathic Pain and Patient-Reported Outcomes in Korean Adults with Chronic Low Back Pain Resulting from Neuropathic Low Back Pain. Asian Spine J 2017;11:917-27.
Sakai Y, Ito K, Hida T, Ito S, Harada A. Neuropathic pain in elderly patients with chronic low back painand effects of pregabalin: a preliminary study. Asian Spine J 2015;9:254-62.
Attal N, Perrot S, Fermanian J, Bouhassira D. The neuropathic components of chronic low back pain: a prospective multicenter study using the DN4 Questionnaire. J Pain 2011;12:1080-7.
Hassan AE, Saleh HA, Baroudy YM, Abdul-Rahman KI, Najjar MW, Kazi MS, et al. Prevalence of neuropathic pain among patients suffering from chronic low back pain in Saudi Arabia. Neurosciences (Riyadh) 2005;10:51-5.
Spahr N, Hodkinson D, Jolly K, Williams S, Howard M, Thacker M. Distinguishing between nociceptive and neuropathic components in chronic low back pain using behavioural evaluation and sensory examination. Musculoskelet Sci Pract 2017;27: 40-48.
Sivas F, Uzun O, Baskan B, Bodur H. The neuropathic pain component among patients with chronic low back-radicular pain. J Back Musculoskelet Rehabil 2018;31:939-46.
Freynhagen R, Baron R, Gockel U, Tolle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 2006;22:1911-20.
Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52.
Gatchel RJ, Mayer T, Dersh J, Robinson R, Polatin P. The association of the SF-36 health status survey with 1-year socioeconomic outcomes in a chronically disabled spinal disorder population. Spine (Phila Pa 1976) 1999;24:2162-70.
Sanjaroensuttikul N. The Oswestry low back pain disability questionnaire (version 1.0) Thai version. J Med Assoc Thai 2007;90:1417-22.
Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain 2001;92:147-57.
Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005;114(1-2):29-36.
Krittayaphong R, Bhuripanyo K, Raungratanaamporn O, Chotinaiwatarakul C, Chaowalit N, Punlee K, et al. Reliability of Thai version of SF-36 questionnaire for the evaluation of quality of life in cardiac patients. J Med Assoc Thai 2000;83 Suppl 2:S130-6.
Andrasinova T, Kalikova E, Kopacik R, Srotova I, Vlckova E, Dusek L, et al. Evaluation of the Neuropathic Component of Chronic Low Back Pain. Clin J Pain 2019;35:7-17.
Li J, He J, Li H, Fan BF, Liu BT, Mao P, et al. Proportion of neuropathic pain in the back region in chronic low back pain patients -a multicenter investigation. Sci Rep 2018;8:16537.
Djordjevic OC, Konstantinovic LM, Miljkovic N. Difference between subjects in early chronic phase of low back pain with and without neuropathic component: observational crosssectional study. Eur J Phys Rehabil Med 2019;55:217-24.
Chaisewikul R, Saejong R, Tongsai S, Thamlikitkul V. Comparative Effectiveness and Safety of Original Gabapentin and Generic Gabapentin in Treating Patients with Neuropathic Pain at Siriraj Hospital, Bangkok, Thailand. Siriraj Med J 2020;64:172-77.
Chaiprateep T, Kolladarungkri T, Kumthornthip W, Hunnangkul S. Effectiveness of Back Exercise and Education for Lower Back Pain Prevention among Nurses at a Tertiary Hospital in Bangkok, Thailand. Siriraj Med J 2020;72:109-16.
Thepsongwat JJ, Supakul R, Panupattanapong S, Witthawaskul J, Cheewakongkiat P, Fongkum W, et al. Effectiveness of the Royal Thai Traditional Massage for Relief of Muscle Pain. Siriraj Med J 2006;58:702-04.
Chatsiricharoenkul S. Single-Blind Randomized Controlled Trial of Poly-Herbal Formula Sahatsatara for Acute Low Back Pain: A Pilot Study. Siriraj Med J 2016; 68:30-36.
Finnerup NB, Haroutounian S, Kamerman P, Baron R, Bennett DLH, Bouhassira D, et al. Neuropathic pain: an updated grading system for research and clinical practice. Pain 2016;157:1599-606.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














