Outcomes of an Early Laparoscopic Cholecystectomy in Acute Cholecystitis, Grades I and II
DOI:
https://doi.org/10.33192/Smj.2022.59Keywords:
Early LC, acute cholecystitis grade I, acute cholecystitis grade IIAbstract
Objective: According to the accumulated benefits of laparoscopic cholecystectomy (LC) in acute cholecystitis (AC), early LC is becoming a standard management for selected patients. While patients with mild AC usually gain the advantages of this approach, removing a more inflamed gallbladder in patients with moderate AC has various results, depending on the institute where the procedure is performed. The aim of the study was to compare the outcomes between early LC in patients with grade I and II AC.
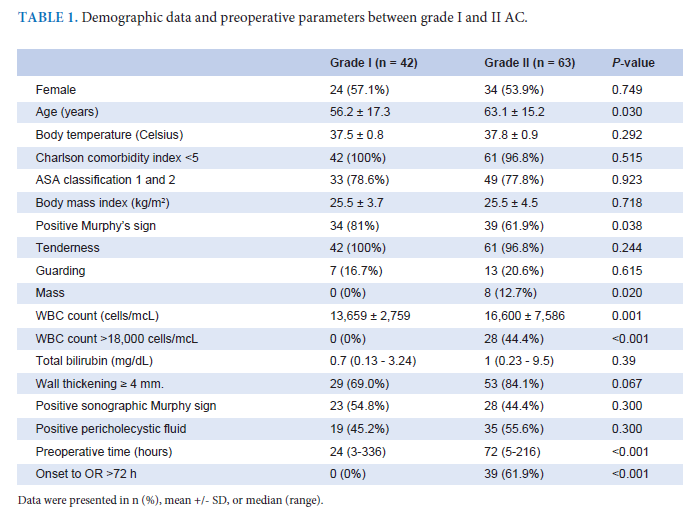
Materials and Methods: From June, 2015 to December, 2019, electronic medical records in the division of Acute Care Surgery at Siriraj Hospital in Bangkok were reviewed retrospectively. An early LC was performed consecutively in 105 cases of AC grades I and II. The overall results and the outcomes comparing grades I and II AC were evaluated.
Results: Forty-two patients were grade I (40%). Patients with grade I AC tended to be younger (56 +/- 17 years vs. 63 +/-15 years, p = 0.03). Among grade II patients, the late onset of more than 72 hours was the most common measure (62%). The estimated blood loss was significantly lower in grade I [30 (5-450) ml. vs. 100 (5-3,000) ml., p =0.018]. The overall conversion rate was 21%, which was significantly higher in grade II AC (28.6% vs. 9.5%, p= 0.026). There were no differences in operating time (125 +/- 47 minutes vs. 117 +/- 44 minutes. p = 0.365), total
lengths of stay [4 (2-7) days vs. 5 (3-28) days, p = 0.163], and post-operative complications (19% vs 25%, p = 0.448). The minor bile duct injuries occurred in four patients (3.8%), 2 cases in each group. From the multivariate analysis, grade II AC did not statistically impact the conversion (adjusted OR 2.99, 95% CI 0.5-17.6, p = 0.225).
Conclusion: Our study shows that the overall and evolving outcomes of early LC for grade I and II AC were safe and feasible. While a higher conversion rate and estimated blood loss attributed to grade II AC, a pre-operative severity grading can guide surgeons to accommodate their ability so as to maximize the benefits of early LC.
References
Wittgen CM, Andrus JP, Andrus CH, Kaminski DL. Cholecystectomy. Which procedure is best for the high-risk patient? Surg Endosc. 1993;7:395-9.
Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, et al. Open versus laparoscopic cholecys-tectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015;18:196-204.
Cao AM, Eslick GD, Cox MR. Early laparoscopic cholecystectomy is superior to delayed acute cholecystitis: a meta-analysis of case-control studies. Surg Endosc. 2016;30(3):1172-82.
Song GM, Bian W, Zeng XT, Zhou JG, Luo YQ, Tian X. Laparoscopic cholecystectomy for acute cholecystitis: early or delayed? Evidence from a systematic review of discordant meta-analyses. Medicine (Baltimore). 2016;95(23):e3835.
Gurusamy KS, Samraj K. Early versus delayed laparoscopic cholecystectomy for acutecholecystitis. Cochrane Da-tabase Syst Rev. 2006;4:CD005440.
Takada T, Kawarada Y, Nimura Y, Yoshida M, Mayumi T, Sekimoto M, et al. Background: Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Surg. 2007;14:1-10.
Kohji O, Kenji S, Tadahiro T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25:55-72.
Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, Kipfmüller K, et al. Acute cholecystitis: early versus de-layed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. 2013;258:385-93.
Ozkardeş AB, Tokaç M, Dumlu EG, Bozkurt B, Ciftçi AB, Yetişir F, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective, randomized study. Int Surg. 2014;99:56-61.
Loozen CS, Blessing MM, van Ramshorst B, van Santvoort HC, Boerma D. The optimal treatment of patients with mild and moderate acute cholecystitis: time for a revision of the Tokyo Guidelines. Surg Endosc. 2017;31(10):3858-63.
Lee W, Kwon J. Delayed laparoscopic cholecytectomy after more than 6 weeks on easily controlled cholecystitis patients. Korean J Hepatobiliary Pancreat Surg. 2013; 17: 60-65.
Inoue K, Ueno T, Douchi D, Shima K, Goto S, Takahashi M, et al. Risk factors for difficulty of laparoscopic cholecystectomy in grade II acute cholecystitis according to the Tokyo guidelines 2013. BMC Surg. 2017;17:114.
Yu-Ning L, Yu-Tung W, Chih-Yuan F, Chien-Hung L, Chi-Tung C, Shang-Yu W, et al. Evaluating the advantages of treating acute cholecystitis by following the Tokyo Guidelines 2018 (TG18): a study emphasizing clin-ical outcomes and medical expenditures. Surg Endosc. [published online: 30 November 2020]. Available from: http://doi.org/10.1007/s00464-020-08162-7
Deeprasertvit A, Deeprasertvit P, Netcharussaeng N. Postoperative Pain Reduction After Additional Intraperitoneal Suction Following Laparoscopic Cholecystectomy: A Prospective Randomized Controlled Study. Siriraj Med J. 2018;70(1):1-5.
Mohamed E, Gianpiero G, Katie T, Sorge R, Al-Hamali S, Ebdewi H. Subtotal Cholecystectomy for “Difficult Gallbladders” Systematic Review and Meta-analysis. JAMA Surg. 2015;150(2):159-68. doi:10.1001/jamasurg.2014.1219
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














