Longus Colli and Vertebral Artery Guide Safety of Cervical Spine Surgery
DOI:
https://doi.org/10.33192/Smj.2022.60Keywords:
Cervical vertebra, uncinate process, anterior cervical surgery, vertebral arteryAbstract
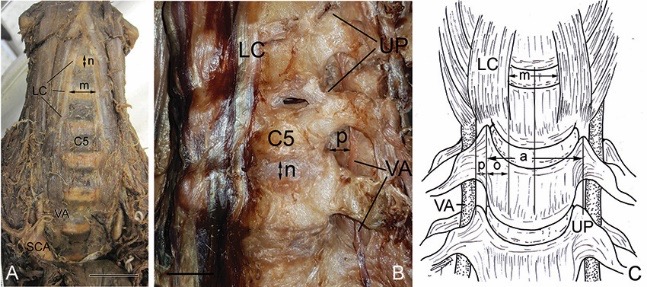
Objective: To improve the safety of the anterior cervical vertebral surgical approach, MRI and CT have been used and the distances between the medial borders of the longus colli (LC) to expose the uncinated process (UP) have been reported. The anatomic parameters of the LC and vertebral artery (VA) were considered here in relation to the UP to minimize complications.
Materials and Methods: Data were obtained from 60 Thai adult skeletons and 20 embalmed cadavers. Direct measurements of the dry cervical vertebrae were performed using digital Vernier calipers, while computer imaging analysis was used for the cadaveric measurements after capturing the images.
Results: No significant difference was noted in the inter-UP distance between the dry and cadaveric cervical measurements. The average UP width was 6.7 ± 0.2 mm. The average distance from the tip of the UP to the VA was 2.6 ± 0.1 mm. The calculated distance from the LC to the UP which derived from the inter-UP distance and the distance between the LC increased from C2 to C7 with an average distance of 11.9 ± 0.3 mm.
Conclusion: Within a distance of 11.9 ± 0.3 mm from the medial border of the LC, UP can be identified. Dissecting at a distance less than 10 mm posterior, 5–6 mm lateral and superior to the base of the UP can avoid VA injury and optimize the safety of the anterior cervical vertebral surgical approach.
References
Hankinson HL, Wilson CB. Use of the operating microscope in anterior cervical discectomy without fusion. J Neurosurg. 1975;43(4):452-6.
Tew JM, Jr., Mayfield FH. Complications of surgery of the anterior cervical spine. Clin Neurosurg. 1976;23:424-34.
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976). 2000;25(8):962-9.
Daentzer D, Deinsberger W, Boker DK. Vertebral artery complications in anterior approaches to the cervical spine: report of two cases and review of literature. Surg Neurol. 2003;59(4):300-9; discussion 9.
Park MS, Moon SH, Kim TH, Oh JK, Kim HJ, Park KT, et al. Surgical anatomy of the longus colli muscle and uncinate process in the cervical spine. Yonsei Med J. 2016;57(4):968-72.
Lu J, Ebraheim NA, Yang H, Skie M, Yeasting RA. Cervical uncinate process: an anatomic study for anterior decompression of the cervical spine. Surg Radiol Anat. 1998;20(4):249-52.
Guvencer M, Men S, Naderi S, Kiray A, Tetik S. The V2 segment of the vertebral artery in anterior and anterolateral cervical spinal surgery: a cadaver angiographic study. Clin Neurol Neurosurg. 2006;108(5):440-5.
Guvencer M, Naderi S, Men S, Sayhan S, Tetik S. Morphometric evaluation of the uncinate process and its importance in surgical approaches to the cervical spine: a cadaveric study. Singapore Med J. 2016;57(10):570-7.
Ebraheim NA, Lu J, Haman SP, Yeasting RA. Anatomic basis of the anterior surgery on the cervical spine: relationships between uncus-artery-root complex and vertebral artery injury. Surg Radiol Anat. 1998;20(6):389-92.
Pait TG, Killefer JA, Arnautovic KI. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Neurosurgery. 1996;39(4):769-76.
Payne EE, Spillane JD. The cervical spine; an anatomicopathological study of 70 specimens (using a special technique) with particular reference to the problem of cervical spondylosis. Brain. 1957;80(4):571-96.
Raykateeraroj N, Kitisin N, Kasemassawachanont A, Porkaew J, Rungruang T, Wunnasinthop S, et al. Morphometric evaluation of the uncinate process of cervical spine for surgical approaches in Thai patients. Siriraj Med J. 2019;71(Suppl 1):S39-44.
Kim SH, Lee JH, Kim JH, Chun KS, Doh JW, Chang JC. Anatomical morphometric study of the cervical uncinate process and surrounding structures. J Korean Neurosurg Soc. 2012;52(4):300-5.
Devin CJ, Kang JD. Vertebral artery injury in cervical spine surgery. Instr Course Lect. 2009;58:717-28.
Peng CW, Chou BT, Bendo JA, Spivak JM. Vertebral artery injury in cervical spine surgery: anatomical considerations, management, and preventive measures. Spine J. 2009;9(1):70-6.
Lu J, Ebraheim NA. The vertebral artery: surgical anatomy. Orthopedics. 1999;22(11):1081-5.
Pangthipampai P, Chinachoti T, Halilamien P, Jirativanont T, Nivatpumin P, Jalayanavin S, et al. Factors Contributing to Delayed Extubation After Cervical Spine Surgery in Siriraj Hospital. Siriraj Med J. 2011;63(4):123-7.
Anastasian ZH, Gaudet JG, Levitt LC, Mergeche JL, Heyer EJ, Berman MF. Factors that correlate with the decision to delay extubation after multilevel prone spine surgery. J Neurosurg Anesthesiol. 2014;26(2):167-71.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














