Factors Predicting Prolonged Postoperative Ileus in Patients Undergoing Major Gastrointestinal Surgery
DOI:
https://doi.org/10.33192/Smj.2022.64Keywords:
Prolonged postoperative ileus, PPOI, major gastrointestinal surgeryAbstract
Objective: This study aimed to investigate the rate of prolonged postoperative ileus (PPOI) and its predictive factors focusing on age, body mass index, smoking status, postoperative mobilization, and preoperative anxiety and depression among patients undergoing major gastrointestinal surgery.
Materials and Methods: This prospective observational study included patients who underwent elective major gastrointestinal surgery in a super tertiary hospital in Thailand. The data were collected using a uniform case record form including the Hospital Anxiety and Depression Scale and Fagerstrom Test for Nicotine Dependence. PPOI was defined using criteria of Vather et al. (2013). Predictive factors for PPOI were determined by multivariate analysis.
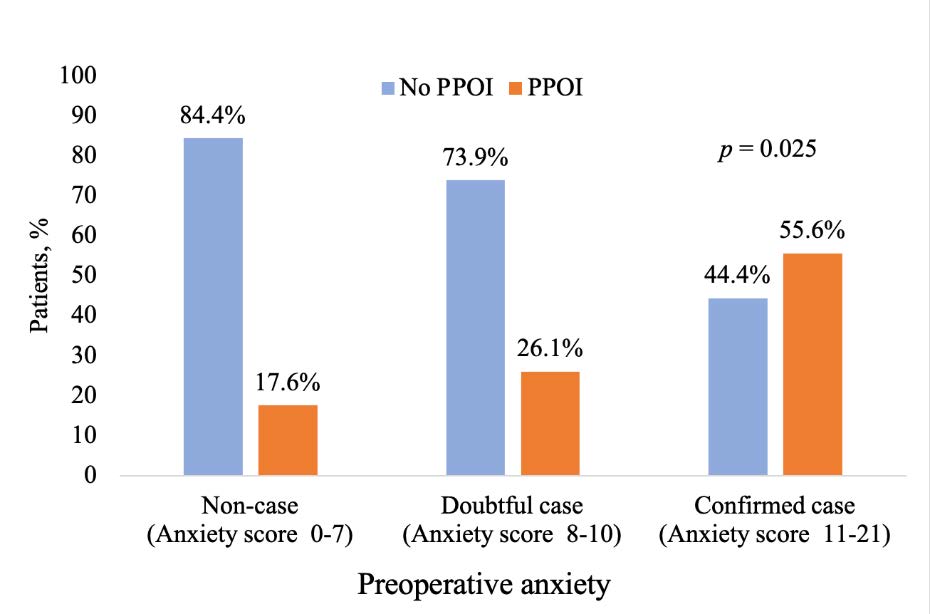
Results: A total of 123 patients were enrolled, with an average age of 59.8 ± 12.7 years. The most common indication for surgery was gastrointestinal malignancy (96 patients, 78%), followed by an open approach (75 patients, 61%) and a combined general and epidural anesthesia (58 patients, 47%). Approximately 30% of patients had a history of smoking. Preoperative anxiety and depression were equally found in nine patients (7%). Twenty-seven patients (22%) experienced PPOI. The significant predictive factors of PPOI were having preoperative anxiety (OR = 6.26, 95% CI = 1.22–44.41, p = 0.046) and being unable to ambulate on postoperative day 1 (OR = 3.26, 95% CI = 1.25–8.50, p = 0.015).
Conclusion: Preoperative anxiety and delayed postoperative ambulation were two predictors for PPOI in this study. Some interventions to reduce preoperative anxiety and encourage early postoperative ambulation should be considered in patients undergoing major elective gastrointestinal surgery.
References
Venara A, Neunlist M, Slim K, Barbieux J, Colas PA, Hamy A, et al. Postoperative ileus: Pathophysiology, incidence, and prevention. J Visc Surg 2016;153(6):439-46.
Bragg D, El-Sharkawy AM, Psaltis E, Maxwell-Armstrong CA, Lobo DN. Postoperative ileus: Recent developments in pathophysiology and management. Clin Nutr (Edinburgh, Scotland) 2015;34(3):367-76.
Holte K, Kehlet H. Postoperative ileus: a preventable event. Br J Surg 2000;87(11):1480-93.
Sugawara K, Kawaguchi Y, Nomura Y, Suka Y, Kawasaki K, Uemura Y, et al. Perioperative Factors predicting prolonged postoperative ileus after Major abdominal surgery. J Gastrointest Surg 2018;22(3):508-15.
Rybakov EG, Shelygin YA, Khomyakov EA, Zarodniuk IV. Risk factors for postoperative ileus after colorectal cancer surgery. Colorectal Dis 2017.
Murphy MM, Tevis SE, Kennedy GD. Independent risk factors for prolonged postoperative ileus development. J Surg Res 2016;201(2):279-85.
Hain E, Maggiori L, Mongin C, Prost AlDJ, Panis Y. Risk factors for prolonged postoperative ileus after laparoscopic sphincter-saving total mesorectal excision for rectal cancer: an analysis of 428 consecutive patients. Surg Endosc 2018;32(1):337-44.
Wolthuis AM, Bislenghi G, Lambrecht M, Fieuws S, de Buck van Overstraeten A, Boeckxstaens G, et al. Preoperative risk factors for prolonged postoperative ileus after colorectal resection. Int J Colorectal Dis 2017;32(6):883-90.
Courtot L, Le Roy B, Memeo R, Voron T, de Angelis N, Tabchouri N, et al. Risk factors for postoperative ileus following elective laparoscopic right colectomy: a retrospective multicentric study. Int J Colorectal Dis 2018;33(10):1373-82.
Alhashemi M, Fiore JF, Jr., Safa N, Al Mahroos M, Mata J, Pecorelli N, et al. Incidence and predictors of prolonged postoperative ileus after colorectal surgery in the context of an enhanced recovery pathway. Surg Endosc 2019;33(7):2313-22.
Rees J, Bobridge K, Cash C, Lyons-Wall P, Allan R, Coombes J. Delayed postoperative diet is associated with a greater incidence of prolonged postoperative ileus and longer stay in hospital for patients undergoing gastrointestinal surgery. Nutr Diet 2018;75(1):24-9.
Vather R, Josephson R, Jaung R, Robertson J, Bissett I. Development of a risk stratification system for the occurrence of prolonged postoperative ileus after colorectal surgery: a prospective risk factor analysis. Surgery 2015;157(4):764-73.
Huang DD, Zhuang CL, Wang SL, Pang WY, Lou N, Zhou CJ, et al. Prediction of prolonged postoperative ileus after radical gastrectomy for gastric cancer: a scoring system obtained from a prospective study. Medicine (Baltimore) 2015;94(51):e2242.
Moghadamyeghaneh Z, Hwang GS, Hanna MH, Phelan M, Carmichael JC, Mills S, et al. Risk factors for prolonged ileus following colon surgery. Surg Endosc 2016;30(2):603-9.
Tevis SE, Carchman EH, Foley EF, Harms BA, Heise CP, Kennedy GD. Postoperative Ileus--More than Just Prolonged Length of Stay? J Gastrointest Surg : official journal of the society for surgery of the alimentary tract 2015;19(9):1684-90.
Kalyanwat A, Jakhar M, Jain S. Postoperative ileus: a study on the role of chewing gum to reduce its duration. Saudi Surg J 2018;6(3):85-8.
Duangchan C, Toskulkao T, Danaidutsadeekul S, Iramaneerat C. Effect of gum chewing on bowel motility in patients with colorectal cancer after open colectomy: A randomized controlled trial. Siriraj Med J 2016;68:135-41.
Dulskas A, Klimovskij M, Vitkauskiene M, Samalavicius NE. Effect of coffee on the length of postoperative ileus after elective laparoscopic left-sided colectomy: a randomized, prospective single-center study. Dis Colon Rectum 2015;58(11):1064-9.
Lohsiriwat V. Mosapride Reduces Prolonged Postoperative Ileus after Open Colorectal Surgery in the Setting of Enhanced Recovery after Surgery (ERAS): A Matched Case-Control Study. Siriraj Med J 2019;71:181-8.
Nematihonar B, Salimi S, Noorian V, Samsami M. Early versus delayed (Traditional) postoperative oral feeding in patients undergoing colorectal anastomosis. Adv Biomed Res 2018;7(1):30.
Manakijsirisuthi W. Early Postoperative Feeding After Gastroduodenal Operation : A 72 Cases Report. Siriraj Med J 2002;54(7):387-93.
Juárez-Parra MA, Carmona-Cantú J, González-Cano JR, Arana-Garza S, Trevino-Frutos RJ. Risk factors associated with prolonged postoperative ileus after elective colon resection. Rev Gastroenterol Mex 2015;80(4):260-6.
Moore BA, Albers KM, Davis BM, Grandis JR, Tögel S, Bauer AJ. Altered inflammatory gene expression underlies increased susceptibility to murine postoperative ileus with advancing age. Am J Physiol Gastrointest Liver Physiol 2007;292(6):G1650-9.
Svatek RS, Fisher MB, Williams MB, Matin SF, Kamat AM, Grossman HB, et al. Age and body mass index are independent risk factors for the development of postoperative paralytic ileus after radical cystectomy. Urology 2010;76(6):1419-24.
Kadota K, Takeshima F, Inoue K, Takamori K, Yoshioka S, Nakayama S, et al. Effects of smoking cessation on gastric emptying in smokers. J clin gastroenterol 2010;44(4):e71-5.
Emmanuel AV, Mason HJ, Kamm MA. Relationship between psychological state and level of activity of extrinsic gut innervation in patients with a functional gut disorder. Gut 2001;49(2):209-13.
Paravati S, Rosani A, Warrington SJ. Physiology, catecholamines. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright© 2020, StatPearls Publishing LLC.; 2020.
Morisawa T, Takahashi T, Nishi S. The effect of a physiotherapy intervention on intestinal motility. J Phys Ther Sci 2015;27(1):165-8.
Nilchaikovit T, Lortrakul M, Phisansuthideth U. Development of Thai version of Hospital Anxiety and Depression Scale in cancer patients. J Psychiatr Assoc Thailand. 1996;41(1):18-30.
Rattanamongkol C, Sindhu S, Toskulkao T, Iramaneerat C. Factors Related to the severity of postoperative complications in patients with primary gastrointestinal (Stomach, Liver, Bile Duct, Colon, and Rectum) cancer. TJNC 2016;31(3):97-109.
Klinsophon T, Janwantanakul P, Thaveeratitham P. Reliability of the Thai version of the Fagerstrom Test for Nicotine Dependence (FTND). J Med Assoc Thai 2017;100(10):1130.
Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg : official journal of the Society for Surgery of the Alimentary Tract 2013;17(5):962-72.
Wolthuis AM, Bislenghi G, Fieuws S, de Buck van Overstraeten A, Boeckxstaens G, D’Hoore A. Incidence of prolonged postoperative ileus after colorectal surgery: a systematic review and meta-analysis. Colorectal Dis 2016;18(1):O1-9.
Abate SM, Chekol YA, Basu B. Global prevalence and determinants of preoperative anxiety among surgical patients: A systematic review and meta-analysis. Int J Surg 2020;25:6-16.
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety 2019;36(1):8-17.
Williams H, Jajja MR, Baer W, Balch GC, Maithel SK, Patel AD, et al. Perioperative anxiety and depression in patients undergoing abdominal surgery for benign or malignant disease. J Surg Oncol 2019;120(3):389-96.
Manabe N, Tanaka T, Hata J, Kusunoki H, Haruma K. Pathophysiology underlying irritable bowel syndrome--from the viewpoint of dysfunction of autonomic nervous system activity. J Smooth Muscle Res = Nihon Heikatsukin Gakkai kikanshi 2009;45(1):15-23.
Mach T. The brain-gut axis in irritable bowel syndrome--clinical aspects. Med Sci Monit 2004;10(6):Ra125-31.
Paine NJ, Watkins LL, Blumenthal JA, Kuhn CM, Sherwood A. Association of depressive and anxiety symptoms with 24-hour urinary catecholamines in individuals with untreated high blood pressure. Psychosom Med 2015;77(2):136-44.
Arı M, Yılmaz E. Impact of pre-operative anxiety on postoperative constipation. Turk J Colorectal Dis 2016;26:39-46.
Stethen TW, Ghazi YA, Heidel RE, Daley BJ, Barnes L, Patterson D, et al. Walking to recovery: the effects of missed ambulation events on postsurgical recovery after bowel resection. J Gastrointest Oncol 2018;9(5):953-61.
Kumar A, Lin L, Bernheim O, Bagiella E, Jandorf L, Itzkowitz SH, et al. Effect of functional status on the quality of bowel preparation in elderly patients undergoing screening and surveillance colonoscopy. Gut Liver 2016;10(4):569-73.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














