Long-Term Rehabilitation Outcomes of Neurological Patients: A Multicenter Study
DOI:
https://doi.org/10.33192/Smj.2022.67Keywords:
Rehabilitation, treatment outcome, inpatients, functions, multicenter studyAbstract
Objective: To evaluate functional outcomes in patients three years after rehabilitation and to identify factors significantly associated with improvement.
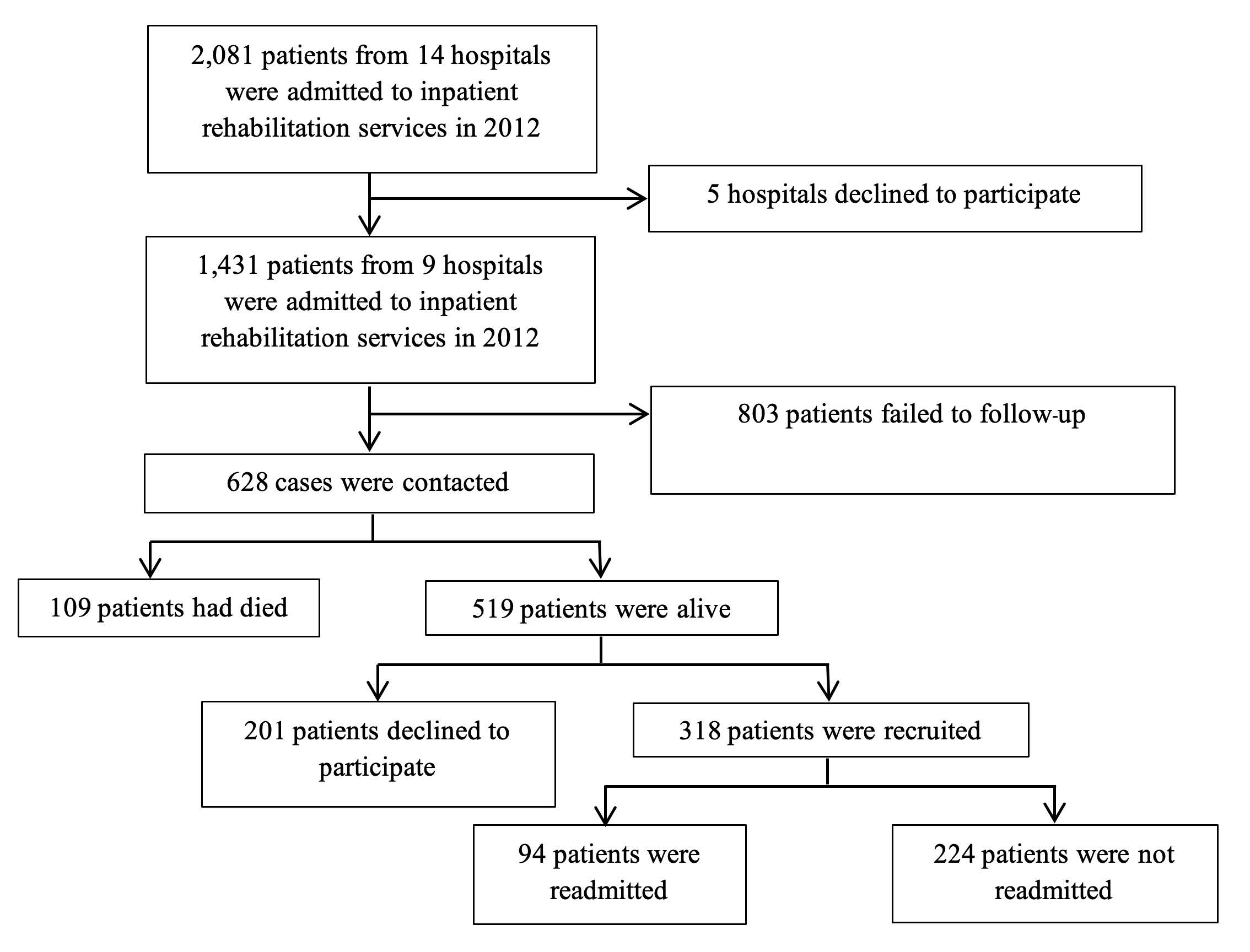
Materials and Methods: This prospective cohort study was carried out in nine tertiary centers to compare functional outcomes (Barthel Index; BI) at discharge with scores at three-year follow-up among various diagnoses and types of admissions. Related factors were evaluated for association with improvement in functional score.
Results: Three hundred and eighteen patients (mean age: 54 years; 60% male) were included. More than half of all patients suffered from a spinal cord injury. After three years, 35% of patients were still receiving physical therapy. Only those who were admitted for intensive rehabilitation showed significant improvement after three years. One hundred and ten patients or 35.8% showed significant improvement over time. A univariate analysis showed type of diagnosis, type of admission, onset to admission interval, BI at discharge, and presence of depression and complications at follow-up to be significantly associated with improvements in functional score in the follow-up period. Using a multivariate analysis, only the type of diagnosis, low BI at discharge, and absence of depression and complications at follow-up related to functional improvement.
Conclusion: One-third of patients had sustained functional improvements from rehabilitation three years after discharge. Participants admitted into intensive rehabilitation showed significant improvements in functional scores between discharge and follow-up. TBI diagnosis, low BI at discharge, absence of depression and complications at follow-up related to long-term functional improvement at the three-year mark.
References
Yee SN, Jung H, San ST, Chek WB, Chiong Y, Lim PAC. Results from a prospective acute inpatient rehabilitation database: Clinical characteristics and functional outcomes using the functional independence measure. Ann Acad Med Singapore. 2007;36:3-10.
Kuptniratsaikul V, Wattanapan P, Wathanadilokul U, Sukonthamarn K, Lukkanapichonchut P, Ingkasuthi K, et al. A Multicenter Study of Efficiency for Rehabilitation Service: A Comparison between Institutes. J Thai Rehabil Med. 2014;24:76-85.
Joa KL, Han TR, Pyun SB, Rah UW, Park JH, Kim YH, et al. Inpatient stroke rehabilitation outcomes in Korea derived from the Korean Brain Rehabilitation Centers’ online database system for the years 2007 to 2011. J Korean Med Sci. 2015;30:644-50.
Turner-Stokes L, Vanderstay R, Stevermuer T, Simmonds F, Khan F, Eagar K. Comparison of rehabilitation outcomes for long term neurological conditions: A cohort analysis of the Australian rehabilitation outcomes centre dataset for adults of working age. PLoS One. 2015;10:e0132275.
Bode RK, Heinemann AW. Course of functional improvement after stroke, spinal cord injury, and traumatic brain injury. Arch Phys Med Rehabil. 2002;83:100-6.
Wang H, Camicia M, Terdiman J, Hung YY, Sandel ME. Time to inpatient rehabilitation hospital admission and functional outcomes of stroke patients. PM R. 2011;3:296-304.
Dijkerman HC, Wood VA, Hewer RL. Long-term outcome after discharge from a stroke rehabilitation unit. J R Coll Physicians Lond. 1996;30:538-46.
Mutai H, Furukawa T, Araki K, Misawa K, Hanihara T. Longterm outcome in stroke survivors after discharge from a convalescent rehabilitation ward. Psychiatry Clin Neurosci. 2013;67:434-40.
Andersen HE, Eriksen K, Brown A, Schultz-Larsen K, Forchhammer BH. Follow-up services for stroke survivors after hospital discharge - A randomized control study. Clin Rehabil. 2002;16:593-603.
Blicher JU, Nielsen JF. Does long-term outcome after intensive inpatient rehabilitation of acquired brain injury depend on etiology? Neuro Rehabilitation. 2008;23:175-83.
Katz DI, Polyak M, Coughlan D, Nichols M, Roche A. Natural history of recovery from brain injury after prolonged disorders of consciousness: outcome of patients admitted to inpatient rehabilitation with 1-4 year follow-up. Prog Brain Res. 2009;177:73-88.
Saifee TA, Kassavetis P, Pareés I, Kojovic M, Fisher L, Morton L, et al. Inpatient treatment of functional motor symptoms: A long-term follow-up study. J Neurol. 2012;259:1958-63.
Whyte J, Nakase-Richardson R, Hammond FM, McNamee S, Giacino JT, Kalmar K, et al. Functional outcomes in traumatic disorders of consciousness: 5-year outcomes from the National Institute on Disability and Rehabilitation Research traumatic brain injury model systems. Arch Phys Med Rehabil. 2013;94:1855-60.
Kuptniratsaikul V, Wattanapan P, Wathanadilokul U, Sukonthamarn K, Lukkanapichonchut P, Ingkasuthi K, et al. The effectiveness and efficiency of inpatient rehabilitation services in Thailand: A prospective multicenter study. Rehabilitation Process and Outcome. 2016;5:13-18.
Collin C, Wade DT, Davies S, Horne V. The barthel ADL index: A reliability study. Disabil Rehabil. 1988;10:61-63.
Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8:46.
Wade DT, Hewer RL. Functional abilities after stroke: Measurement, natural history and prognosis. J Neurol Neurosurg Psychiatry. 1987;50:177-82.
Kuptniratsaikul V, Kovindha A, Piravej K, Dajpratham P. First-Year Outcomes after Stroke Rehabilitation: A Multicenter Study in Thailand. ISRN Rehabilitation. 2013;2013: 1-6.
Pattanasuwanna P, Kuptniratsaikul V. Inpatient rehabilitation outcomes in patients with stroke at Thailand’s largest tertiary referral center : A 5-year retrospective study. J Sci Res Stud. 2017;4:208-16.
Rinkaewkan P, Kuptniratsaikul V. The effectiveness of inpatients rehabilitation for spinal cord patients in Siriraj hospital. Spinal Cord. 2015;53:591-7.
Willemse-van Son AHP, Ribbers GM, Verhagen AP, Stam HJ. Prognostic factors of long-term functioning and productivity after traumatic brain injury: a systematic review of prospective cohort studies. Clin Rehabil. 2007;21:1024-37.
Hankey GJ, Jamrozik K, Broadhurst RJ, Forbes S, Anderson CS. Long-term disability after first-ever stroke and related prognostic factors in the Perth Community Stroke Study, 1989-1990. Stroke. 2002;33:1034-40.
Musicco M, Emberti L, Nappi G, Caltagirone C. Early and long-term outcome of rehabilitation in stroke patients: The role of patient characteristics, time of initiation, and duration of interventions. Arch Phys Med Rehabil. 2003;84:551-58.
Meyer MJ, Pereira S, McClure A, Teasell R, Thind A, Koval J, et al. A systematic review of studies reporting multivariable models to predict functional outcomes after post-stroke inpatient rehabilitation. Disabil Rehabil. 2015;37:1316-23.
Mutai H, Furukawa T, Nakanishi K, Hanihara T. Longitudinal functional changes, depression, and health-related quality of life among stroke survivors living at home after inpatient rehabilitation. Psychogeriatrics. 2016;16:185-90.
Pohjasvaara T, Vataja R, Leppävuori A, Kaste M, Erkinjuntti T. Depression is an independent predictor of poor long-term functional outcome post-stroke. Eur J Neurol. 2001;8:315-9.
Thanakiatpinyo T, Dajpratham P, Kovindha A, Kuptniratsaikul V. Quality of life of stroke patients at one year after discharge from inpatient rehabilitation: A multicenter study. Siriraj Med J. 2021;73:253-60.
Kuptniratsaikul V, Thitisakulchai P, Sarika S Khaewnaree S. The burden of stroke on caregivers at 1-year period: a multicenter study. J Thai Rehabil Med. 2018;28:8-14.
Graham JE, Granger C V., Karmarkar AM, Deutsch A, Niewczyk P, Divita MA, et al. The uniform data system for medical rehabilitation: Report of follow-up information on patients discharged from inpatient rehabilitation programs in 2002-2010. Am J Phys Med Rehabil. 2014;93:231-44.
Ottenbacher KJ, Karmarkar A, Graham JE, Kuo YF, Deutsch A, Reistetter TA, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service medicare patients. JAMA 2014;311:604-14.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














