Malignancy of the Lymph Node: How General Practitioners and Pathologists can achieve a Definitive Diagnosis
DOI:
https://doi.org/10.33192/Smj.2022.72Keywords:
Lymph node, malignancy, multimodality, morphology, immunohistochemistry, pathologic diagnosisAbstract
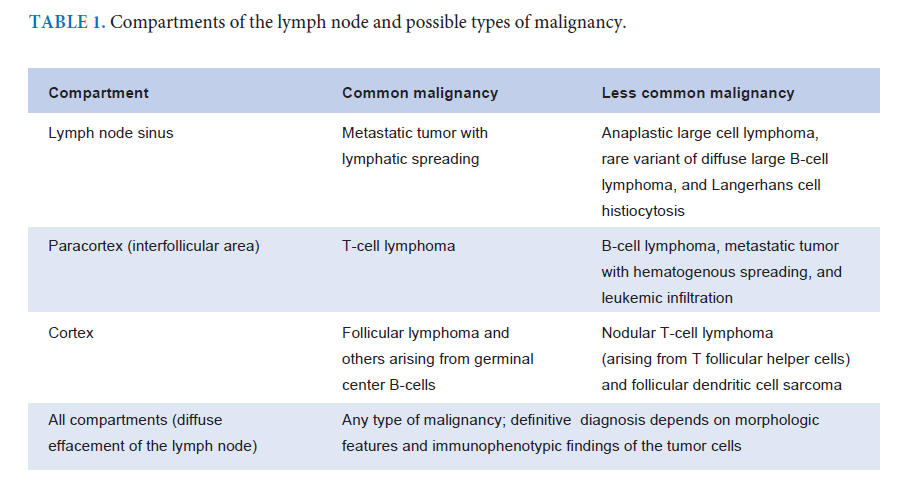
The lymph node plays an important role in the lymphatic spread of abnormal antigens from exogenous or endogenous sources, including infectious agents, foreign bodies, self-antigens, and malignant cells, by harboring various immune cells that react to abnormal antigens and their sources. This often leads to enlargement of the lymph node, also known as “lymphadenopathy.” In this review article, malignancy of the lymph node is the main focus, especially regarding how general practitioners and pathologists can achieve a definitive diagnosis. The basic principle relies on the normal structure, cellular components, and functions of the lymph node as well as the types of malignancy found. Careful clinical history taking of any possible cause of lymphadenopathy warrants exclusion of any mimics of malignancy of the lymph node, including drug reactions and immunodeficiency states. An adequate cell or tissue sample allows pathologists to work efficiently by mastering the multimodality approach under good clinical collaboration. Effective communication between pathologists and physicians regarding relevant laboratory investigations should make it easier to diagnose a specific type of malignancy. This review article also focuses on how general pathologists handle cell or tissue samples by conventional morphologic evaluation and panels of immunohistochemistry so that general practitioners understand the diagnostic process and understand how to diagnose malignancy of the lymph node.
References
Sakai O, Curtin HD, Romo LV, Som PM. Lymph node pathology. Benign proliferative, lymphoma, and metastatic disease. Radiol Clin North Am. 2000;38:979-98, x.
Billström R, Ahlgren T, Békássy AN, Malm C, Olofsson T, Höglund M, et al. Acute myeloid leukemia with inv(16)(p13q22): involvement of cervical lymph nodes and tonsils is common and may be a negative prognostic sign. Am J Hematol. 2002;71:15-9.
Skoog L, Tani E. Lymphoma look-alike. Monogr Clin Cytol. 2009;18:64-75.
Devoe K, Weidner N. Immunohistochemistry of small roundcell tumors. Semin Diagn Pathol. 2000;17:216-24.
Swerdlow SH, Campo E, Harris NL, et al. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues (Revised 4th edition). Lyon: IARC; 2017.
Sukpanichnant S, Oo WM. Incidental Malignant Lymphoma and Lymphoproliferative Disorders in Lymph Node Dissection Specimens during Tumor Removal in Various Organs. Siriraj Med J. 2020;72:103-8.
Mihm Jr MC, Mulé JJ. Reflections on the Histopathology of Tumor-Infiltrating Lymphocytes in Melanoma and the Host Immune Response. Cancer Immunol Res. 2015;3:827-35.
Hendry S, Salgado R, Gevaert T, Russell PA, John T, Thapa B, et al. Assessing Tumor-infiltrating Lymphocytes in Solid Tumors: A Practical Review for Pathologists and Proposal for a Standardized Method From the International Immunooncology Biomarkers Working Group: Part 1: Assessing the Host Immune Response, TILs in Invasive Breast Carcinoma and Ductal Carcinoma In Situ, Metastatic Tumor Deposits and Areas for Further Research. Adv Anat Pathol. 2017;24:235-51.
Hendry S, Salgado R, Gevaert T, Russell PA, John T, Thapa B, et al. Assessing Tumor-Infiltrating Lymphocytes in Solid Tumors: A Practical Review for Pathologists and Proposal for a Standardized Method from the International Immuno-Oncology Biomarkers Working Group: Part 2: TILs in Melanoma, Gastrointestinal Tract Carcinomas, Non-Small Cell Lung Carcinoma and Mesothelioma, Endometrial and Ovarian Carcinomas, Squamous Cell Carcinoma of the Head and Neck, Genitourinary Carcinomas, and Primary Brain Tumors. Adv Anat Pathol. 2017;24:311-35.
Owattanapanich W, Phoompoung P, Sukpanichnant S. ALKpositive anaplastic large cell lymphoma undiagnosed in a patient with tuberculosis: a case report and review of the literature. J Med Case Rep 2017;11:132.
Leatham EW, Eeles R, Sheppard M, Moskovic E, Williams MP, Horwich A, et al. The association of germ cell tumours of the testis with sarcoid-like processes. Clin Oncol (R Coll Radiol). 1992;4:89-95.
Brunner A, Kantner J, Tzankov A. Granulomatous reactions cause symptoms or clinically imitate treatment resistance in small lymphocytic lymphoma/chronic lymphocytic leukaemia more frequently than in other non-Hodgkin lymphomas. J Clin Pathol. 2005;58:815-9.
Jiang XS, West DS, Lagoo AS. Lymph node infarction: role of underlying malignancy, tumour proliferation fraction and vascular compromise--a study of 35 cases and a comprehensive review of the literature. Histopathology. 2013;62:315-25.
Tokuhira M, Tamaru JI, Kizaki M. Clinical management for other iatrogenic immunodeficiency-associated lymphoproliferative disorders. J Clin Exp Hematop. 2019;59:72-92.
Wei S, Henderson-Jackson E, Qian X, Bui MM. Soft Tissue Tumor Immunohistochemistry Update: Illustrative Examples of Diagnostic Pearls to Avoid Pitfalls. Arch Pathol Lab Med. 2017;141:1072-91.
Blazer DG 3rd, Sabel MS, Sondak VK. Is there a role for sentinel lymph node biopsy in the management of sarcoma? Surg Oncol. 2003;12:201-6.
Ahn D, Lee GJ, Sohn JH, Jeong JY. Fine-needle aspiration cytology versus core-needle biopsy for the diagnosis of extracranial head and neck schwannoma. Head Neck. 2018;40:2695-2700.
Garin-Chesa P, Fellinger EJ, Huvos AG, Beresford HR, Melamed MR, Triche TJ, et al. Immunohistochemical analysis of neural cell adhesion molecules. Differential expression in small round cell tumors of childhood and adolescence. Am J Pathol. 1991;139:275-86.
Gurel B, Ali TZ, Montgomery EA, Begum S, Hicks J, Goggins M, et al. NKX3.1 as a marker of prostatic origin in metastatic tumors. Am J Surg Pathol. 2010;34:1097-105.
McDonnell JM, Beschorner WE, Kuhajda FP, deMent SH. Common leukocyte antigen staining of a primitive sarcoma. Cancer. 1987;59:1438-41.
Nandedkar MA, Palazzo J, Abbondanzo SL, Lasota J, Miettinen M. CD45 (leukocyte common antigen) immunoreactivity in metastatic undifferentiated and neuroendocrine carcinoma: a potential diagnostic pitfall. Mod Pathol. 1998;11:1204-10.
Houreih MA, Eyden BP, Reeve N, Banerjee SS. Aberrant leukocyte common antigen expression in metastatic small cell lung carcinoma: a rare finding and a potential diagnostic pitfall. Appl Immunohistochem Mol Morphol. 2007;15:236-8.
Ngo N, Patel K, Isaacson PG, Naresh KN. Leucocyte common antigen (CD45) and CD5 positivity in an "undifferentiated" carcinoma: a potential diagnostic pitfall. J Clin Pathol. 2007;60:936-8.
Gasljevic G, Matter MS, Blatnik O, Unk M, Dirnhofer S. NUT Carcinoma: A Clinical, Morphological and Immunohistochemical Mimicker-The Role of RNA Sequencing in the Diagnostic Procedure. Int J Surg Pathol. 2022;30:273-7.
Jones H, Anthony PP. Metastatic prostatic carcinoma presenting as left-sided cervical lymphadenopathy: a series of 11 cases. Histopathology. 1992;21:149-54.
Huey RW, Smaglo BG, Estrella JS, Matamoros A, Overman MJ, Varadhachary GR, et al. Cancer of Unknown Primary Presenting as Bone-Predominant or Lymph Node-Only Disease: A Clinicopathologic Portrait. Oncologist. 2021;26:e650-7.
Ouldamer L, Cayrol M, Vital M, Fièvre C, Druelles M, Arbion F, et al. Axillary lymph node metastases from unknown primary: A French multicentre study. Eur J Obstet Gynecol Reprod Biol. 2018;223:103-7.
Shao Y, Liu X, Hu S, Zhang Y, Li W, Zhou X, et al. Sentinel node theory helps tracking of primary lesions of cancers of unknown primary. BMC Cancer. 2020;20:639.
Pena GP, Andrade-Filho JS. How does a pathologist make a diagnosis? Arch Pathol Lab Med 2009;133:124-32.
Middleton LP, Feeley TW, Albright HW, Walters R, Hamilton SH. Second-opinion pathologic review is a patient safety mechanism that helps reduce error and decrease waste. J Oncol Pract. 2014;10:275-80.
Bellizzi AM. An Algorithmic Immunohistochemical Approach to Define Tumor Type and Assign Site of Origin. Adv Anat Pathol. 2020;27:114-63.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














