Predicting the Need for Continuation of N-acetylcysteine Treatment among Acute Paracetamol Overdose Patients with Psi Parameter
DOI:
https://doi.org/10.33192/Smj.2022.77Keywords:
Paracetamol, acute liver injury, N-acetylcysteine, prognosis, psi IntroductionAbstract
Objective: AcetaCalc was used to evaluate Psi’s accuracy in predicting cases that required prolonged NAC therapy, as well as Psi’s optimal cut-off.
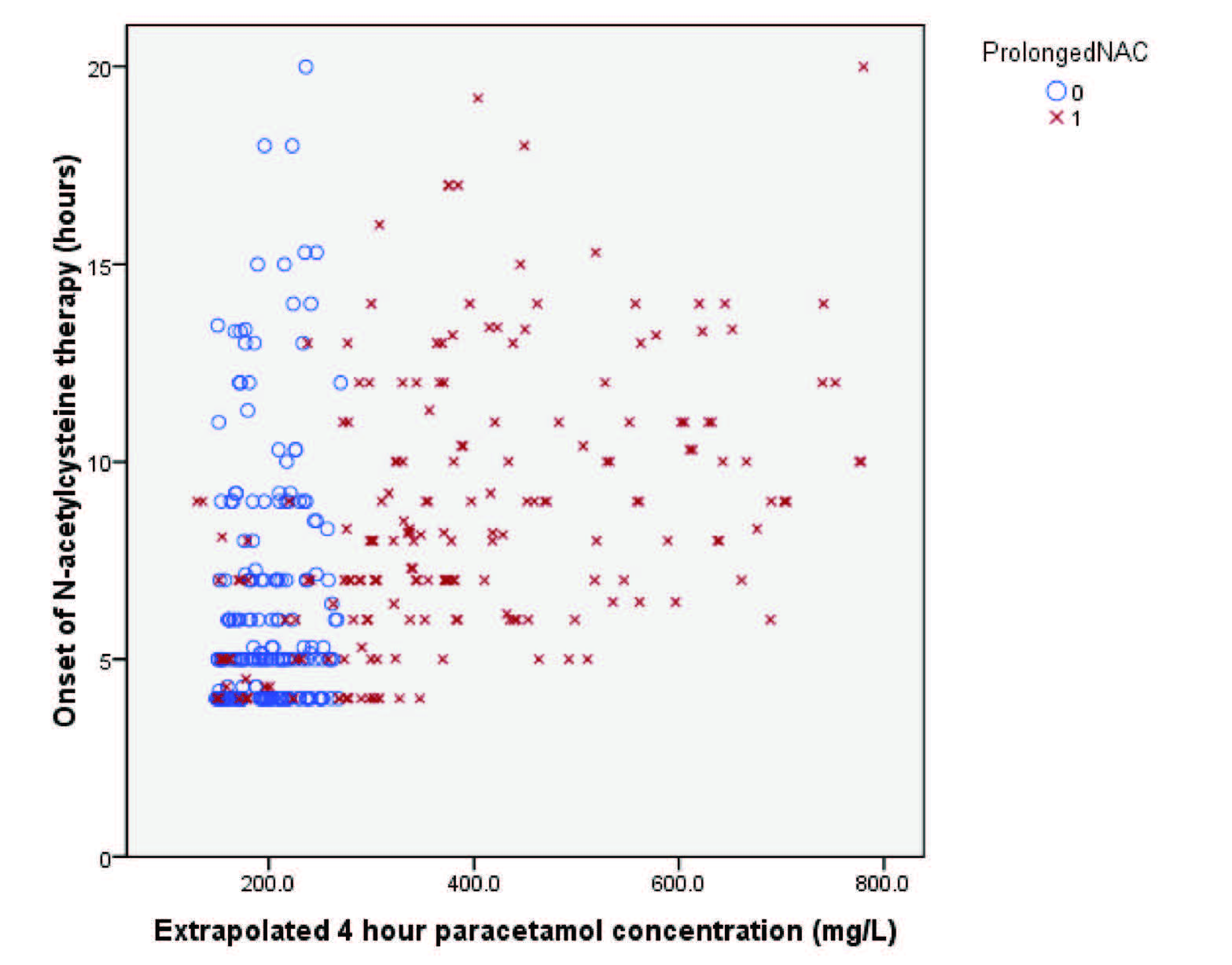
Materials and Methods: This is a retrospective study of patients with acute paracetamol overdose who were treated with NAC at Siriraj Hospital between 2007 and 2016. The Psi parameter was calculated using the Acetacalc after entering paracetamol concentrations, blood sampling times, and NAC onset times. Indications for NAC continuation is in accordance with the guidelines, which recommended that NAC treatment be continued if the follow-up aminotransferase reached 50 U/L or higher.
Results: We enrolled 403 patients, the proportion of NAC prolongation was 50.4 %. Psi was shown to be a significant predictor of NAC prolongation (p < 0.001) with area under the receiver operational characteristics curve 0.766 (95% confidence interval (CI) 0.719-0.813). The Psi cutoff with highest Youden index was 1.757 mM-hour. The sensitivities and specificities of the cutoff were 0.517 (95% CI 0.449-0.585) and 0.940 (95% CI 0.898-0.965), respectively.
Conclusion: Psi parameter calculated through AcetaCalc is a useful tool for the prediction of cases where extension of NAC therapy beyond the standard regimen is indicated.
References
Chiew AL, Buckley NA. Acetaminophen Poisoning. Crit Care Clin. 2021;37(3):543-61.
Rumack BH. Acetaminophen hepatotoxicity: the first 35 years. J Toxicol Clin Toxicol. 2002;40(1):3-20.
Harrison PM, Keays R, Bray GP, Alexander GJ, Williams R. Improved outcome of paracetamol-induced fulminant hepatic failure by late administration of acetylcysteine. Lancet. 1990;335(8705):1572-3.
Keays R, Harrison PM, Wendon JA, Forbes A, Gove C, Alexander GJ, et al. Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial. Bmj. 1991;303(6809):1026-9.
Chiew AL, Reith D, Pomerleau A, Wong A, Isoardi KZ, Soderstrom J, et al. Updated guidelines for the management of paracetamol poisoning in Australia and New Zealand. Med J Aust. 2020;212(4):175-83.
Curtis RM, Sivilotti ML. A descriptive analysis of aspartate and alanine aminotransferase rise and fall following acetaminophen overdose. Clin Toxicol (Phila). 2015;53(9):849-55.
Wong A, Graudins A. Risk prediction of hepatotoxicity in paracetamol poisoning. Clin Toxicol (Phila). 2017;55(8):879-92.
Chomchai S, Chomchai C, Anusornsuwan T. Acetaminophen psi parameter: a useful tool to quantify hepatotoxicity risk in acute acetaminophen overdose. Clin Toxicol (Phila). 2011;49(7):664-7.
Sivilotti ML, Good AM, Yarema MC, Juurlink DN, Johnson DW. A new predictor of toxicity following acetaminophen overdose based on pretreatment exposure. Clin Toxicol (Phila). 2005;43(4):229-34.
Chomchai S, Lawattanatrakul N, Chomchai C. Acetaminophen Psi Nomogram: a sensitive and specific clinical tool to predict hepatotoxicity secondary to acute acetaminophen overdose. J Med Assoc Thai. 2014;97(2):165-72.
Sivilotti ML, Yarema MC, Juurlink DN, Good AM, Johnson DW. A risk quantification instrument for acute acetaminophen overdose patients treated with N-acetylcysteine. Ann Emerg Med. 2005;46(3):263-71.
Chomchai S, Chomchai C. Predicting acute acetaminophen hepatotoxicity with acetaminophen-aminotransferase multiplication product and the Psi parameter. Clin Toxicol (Phila). 2014;52(5):506-11.
Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644-7.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373-9.
Cairney DG, Beckwith HK, Al-Hourani K, Eddleston M, Bateman DN, Dear JW. Plasma paracetamol concentration at hospital presentation has a dose-dependent relationship with liver injury despite prompt treatment with intravenous acetylcysteine. Clin Toxicol (Phila). 2016;54(5):405-10.
Chiew AL, Gluud C, Brok J, Buckley NA. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2018;2(2):Cd003328.
Chomchai S, Mekavuthikul P, Phuditshinnapatra J, Chomchai C. Sensitivity of dose-estimations for acute acetaminophen overdose in predicting hepatotoxicity risk using the Rumack-Matthew Nomogram. Pharmacol Res Perspect. 2022;10(1):e00920.
Hoegberg LCG, Shepherd G, Wood DM, Johnson J, Hoffman RS, Caravati EM, et al. Systematic review on the use of activated charcoal for gastrointestinal decontamination following acute oral overdose. Clin Toxicol (Phila). 2021;59(12):1196-227.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














