Comparative Study Regarding Autonomy of Final-Year Surgical Residents: A Case Study of Perception among Surgical Residents, Surgical Staff, Administrators, and Patients at Siriraj University Hospital
DOI:
https://doi.org/10.33192/Smj.2022.75Keywords:
Autonomy, independence, resident, surgeryAbstract
Objective: To identify barriers towards resident autonomy as perceived through four groups; surgical residents, surgical staff, administrators, and patients.
Materials and Methods: Anonymous surveys were distributed to these four groups. Data were thematically analyzed.
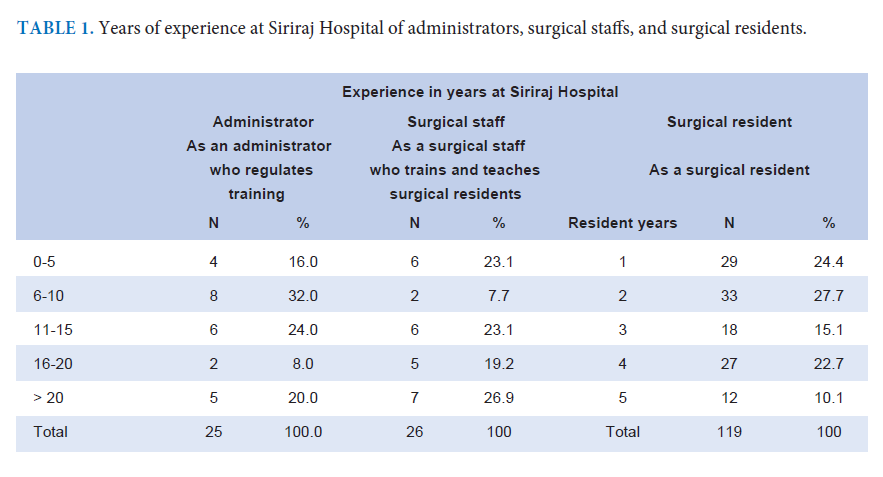
Results: 401 responses were collected including 231 patients. The response rate of residents, surgical staff, and administrators was 62.2% (119), 44.8% (26), and 43.1% (25) respectively. Patients had more favorable views of resident participation than administrators and surgical staff. Administrators and surgical staff indicated that residents have a positive effect on overall quality of care provided and so do the patients, however, administrators and surgical staff believed that too much autonomy for a resident deceased patient safety. When resident autonomy increased, increased cost of patient care was considered. Residents and patients have the same opinion that patients should receive a discount on medical expenses, which is opposite to administrators’ and surgical staff’s opinion.
The presence of surgical staff in the operation room had a major impact on resident autonomy and a big influence on patient acceptance of operative complications. Even in complicated operations, most patients felt comfortable having a resident perform on with surgical staff controlling the operation. Surgical staff provided too much direction in either patient care or operation and did not take residents’ input as seriously as expected and seldom explained the reasons before changing treatment regimens.
Conclusion: Surgical residents, surgical staff, and patients had discordant perceptions of resident autonomy in many aspects. Self-determination theory should be applied. Scaffolding strategy, mentoring program would be the solutions.
References
Iramaneerat C, Rangsisombatsiri C. Satisfaction Survey of Graduates from the Doctor of Medicine Program of the Faculty of Medicine Siriraj Hospital. Siriraj Med Bull. 2010;3:2.
Lertrattananon D, Limsawart W, Dellow A, Pugsley. Does medical training in Thailand prepare doctors for work in community hospitals? An analysis of critical incidents. Human Resources for Health. 2019;17(62):1-8.
Lewis FR, Klingensmith ME. Issues in general surgery residency training. Ann Surg. 2012;256(4):553-9.
Sterkenburg A, Barach P, Kalkman C, Gielen M, Cate OT. When do supervising physicians decide to entrust residents with unsupervised tasks? Acad Med. 2010;85(9):1408-17.
Kempenich JW, Willis RE, Rakosi R, Wiersch J, Schenarts P. How do perceptions of autonomy differ in general surgery training between faculty, senior residents, hospital administrators, and the general public? A multi-institutional study. J Surg Educ. 2015:72(6):193-201.
Biondi EA, Varade WS, Garfunkel LC, Lynn JF, Craig MS, Cellini MM, et al. Discordance between resident and faculty perceptions of resident autonomy: Can Self Determination Theory help interpret differences and guided strategies for bridging the divide? Acad Med. 2015;90:462-71.
Teman NR, Gauger PG, Mullan PB, Tarpley JL, Minter RM. Entrustment of general surgery residents in the operating room: factors contributing to provision-of resident autonomy. J Am Coll Surg. 2014;219(4):778-87.
Cate OT. Trust, competence, and the supervisor’s role in postgraduate training. BMJ. 2006;333(7571):748-51.
Chalabian J, Bremner R. The effects of programmatic change on resident motivation. Surgery. 1998;123(5):511-7.
Santry HP, Chokshi N, Datrice N, Guitron J, Moller MG. General surgery training and the demise of the general surgeon. Bull Am Coll Surg. 2008;93(7):32-8.
Arriaga AF, Elbardissi AW, Regenbogen SE, Green- berg CC, Berry WR, Lipsitz S. A policy-based intervention for the reduction of communication breakdowns in inpatient surgical care: results from a Harvard surgical safety collaborative. Ann Surg. 2011;253(5):849-54.
Babbott S. Commentary: watching closely at a distance: key tensions in supervising resident physicians. Acad Med. 2010;85(9):1399-400.
Phitayakorn R, Williams RG, Yudkowsky R, Harris IB, Hauge LS, Widmann WD, et al. Patient-care-related telephone communication between general surgery residents and attending surgeons. J Am Coll Surg. 2008;206(4):742-50.
Kim HN, Gates E, Lo B. What hysterectomy patients want to know about the roles of residents and medical students in their care. Acad Med. 1998;73(3):339-41.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68-78.
Williams GC, Deci EL. The importance of supporting autonomy in medical education. Ann Intern Med. 1998;129:303-8.
Kusurkar R, Cate OT. AM last page: education is not filling a bucket, but lighting a fire: self-determination theory and motivation in medical students. Acad Med. 2013;88(6):904.
Greene FL. Transition to practice: a bold move. General Surgery News. 2013;40(N3):1.
Castleberry AW, Clary BM, Migaly J, Worni M, Ferranti JM, Pappas TN, et al. Resident education in the era of patient safety: a nationwide analysis of outcomes and complications in residentassisted oncologic surgery. Ann Surg Oncol. 2013;20(12):3715-24.
Hernandez-Irizarry R, Zendejas B, Ali SM, Lohse CM, Farley DR. Impact of resident participation on laparoscopic inguinal hernia repairs: are residents slowing us down? J Surg Educ. 2012;69(6):746-52.
Reichgott MJ, Schwartz JS. Acceptance by private patients of resident involvement in their outpatient care. J Med Educ. 1983;58(9):703-9.
Watson Wyatt Worldwide. Work USA 2000: Employee commitment and the bottom line. Bethesda, MD: Watson Wyatt Worldwide. 2000.
Javidan M, Dorfman PW, Sully de Luque M, House RJ. In the eye of the beholder: Cross cultural lessons in leadership from project GLOBE. Academic of Management Perspectives. 2006;2:67-90.
Niljaeng N, Pruetipibultham O. An examination of the relationships of global leadership competency, trust in leader, and team process effectiveness in Thailand. Human Resource and Organization Development Journal. 2018;10(1):2-33.
Dirks KT. Trust in leadership and team performance: evidence from NCAA basketball. J Appl Psychol. 2000;85(6):1004-12.
Fulmer CA, Gelfand MJ. At what level (and in whom) we trust: Trust across multiple organizational level. Journal of Management. 2012;38:1167-230.
Wu JT, Wahab MT, Ikbal MF, Loo TWW, Kanesvaran R, Radha Krishna LK. Toward an interprofessional mentoring program in palliative care - a review of undergraduate and postgraduate mentoring in medicine, nursing, surgery and social work. J Palliat Care Med. 2016;6:292.
Ramanan RA, Taylor WC, Davis RB, Phillips RS. Mentoring matters. Mentoring and career preparation in internal medicine residency training. J Gen Intern Med. 2006;21:340-5.
Dimitriadis K, Borch PVD, Störmann S, Meinel FG, Moder S, Reincke M, et al. Characteristics of mentoring relationships formed by medical students and faculty. Med Educ Online, 2012:1(17):242.
Yehia BR, Cronholm PF, Wilson N, Palmer SC, Sisson SD, Guilliames CE, et al. Mentorship and pursuit of academic medicine careers: a mixed methods study of residents from diverse backgrounds. BMC Med Educ. 2014;14:26.
Eckleberry-Hunt J, Tucciarone J. The challenges and opportunities of teaching “Generation Y”. J Grad Med Educ. 2011;3:458-61.
Shangraw RE, Whitten CW. Managing intergenerational differences in academic anesthesiology. Curr Opin Anaesthesiol. 2007;20:558-63.
Eva KW, Regehr G. Self-assessment in the health professions: A reformulation and research agenda. Acad Med. 2005;80(10 Suppl):S46-S54.
Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA. 2006;296:1094-102.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














