Survival Analysis of and Prognostic Factors for Metastatic Epidural Spinal Cord Compression Compared between Preoperative Known and Unknown Primary Tumors
Keywords:
Metastasis, spinal cord compression, unknown primary tumor, survival time, prognosis, urgency decompressionAbstract
Objective: To analyze the median survival time of and prognostic factors for metastatic epidural spinal cord compression (MESCC) secondary to preoperative unknown primary tumor (pre-op UPT) compared to MESCC secondary to preoperative known primary tumor (pre-op KPT).
Materials and Methods: This retrospective cohort study reviewed all consecutive MESCC patients who underwent surgical decompression with or without stabilization within 72 hours of admission during 2010 to 2016. Survival was compared between the pre-op UPT and pre-op KPT groups, and preoperative and postoperative prognostic factors for survival were analyzed.
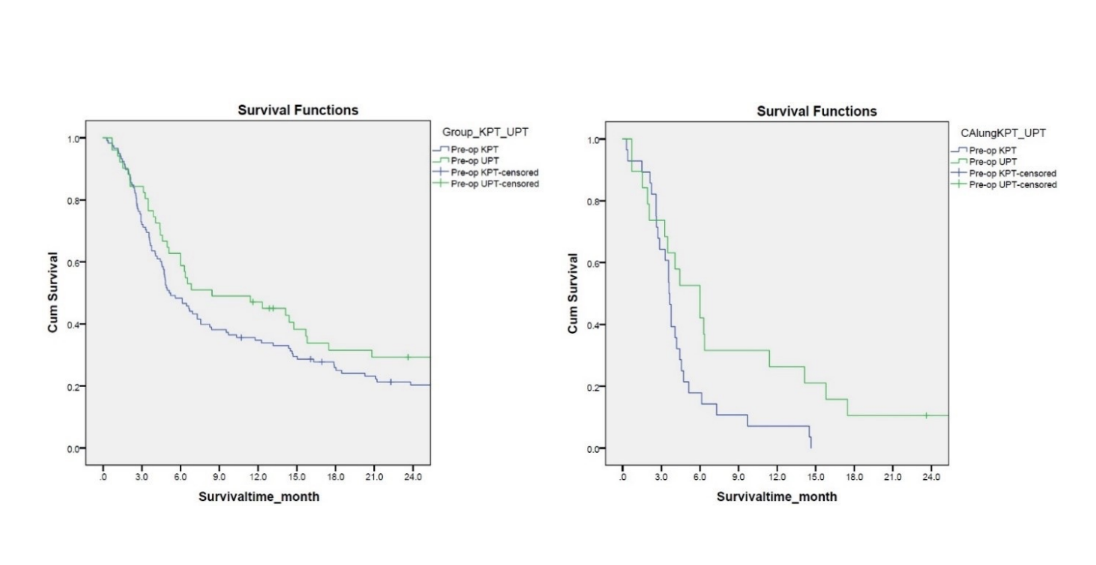
Results: A total of 169 patients (pre-op UPT: 51, and pre-op KPT: 118) were enrolled. The survival rate at 3, 6, and 12 months was 84.3%, 58.8%, and 47.1% in the pre-op UPT group, and 72.0%, 48.3%, and 34.7% in the pre-op KPT group, respectively. The median survival time secondary to lung cancer was significantly longer in the pre-op UPT group (6.0±1.4 months) than in the pre-op KPT group (3.6±0.2 months) (p=0.031). Multivariate analysis revealed survival time to be influenced by preoperative known or unknown primary tumor status, revised Tokuhashi score, the adjuvant therapy, and postoperative complications, including myocardial infarction, gastrointestinal bleeding, and urinary tract infection.
Conclusion: MESCC secondary to preoperative unknown primary tumor patients who had the clinical presentation with acute progressive neurological deficits who need urgency spine surgery has comparable survival to MESCCsecondary to preoperative known primary tumors.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69(1):7-34.
Rose PS, Buchowski JM. Metastatic disease in the thoracic and lumbar spine: evaluation and management. J Am Acad Orthop Surg 2011;19(1):37-48.
Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus 2001;11(6):e10.
Furstenberg CH, Wiedenhofer B, Gerner HJ, Putz C. The effect of early surgical treatment on recovery in patients with metastatic compression of the spinal cord. J Bone Joint Surg Br 2009;91(2):240-4.
Chavasiri C, Sukprasert N, Chavasiri S. Depression, Social Support, and Coping Stratergies in Individuals with Spinal Injury Depression with Spinal Injury Patients. Siriraj Med J 2021;73(8):518-25.
Metastatic Spinal Cord Compression: Diagnosis and Management of Patients at Risk of or with Metastatic Spinal Cord Compression. Cardiff (UK); 2008.
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2001;26(3):298-306.
Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005;30(19):2186-91.
Tokuhashi Y, Uei H, Oshima M, Ajiro Y. Scoring system for prediction of metastatic spine tumor prognosis. World J Orthop 2014;5(3):262-71.
Bollen L, Dijkstra SPD, Bartels R, Graeff A, Poelma DLH, Brouwer T, et al. Clinical management of spinal metastases. The Dutch national guideline. Eur J Cancer 2018;104:81-90.
Yalamanchili M, Lesser GJ. Malignant spinal cord compression. Curr Treat Options Oncol 2003;4(6):509-16.
Hosono N, Ueda T, Tamura D, Aoki Y, Yoshikawa H. Prognostic relevance of clinical symptoms in patients with spinal metastases. Clin Orthop Relat Res 2005;(436):196-201.
Pointillart V, Vital JM, Salmi R, Diallo A, Quan GM. Survival prognostic factors and clinical outcomes in patients with spinal metastases. J Cancer Res Clin Oncol 2011;137(5):849-56.
Tatsui CE, Suki D, Rao G, Kim SS, Salaskar A, Hatiboglu MA, et al. Factors affecting survival in 267 consecutive patients undergoing surgery for spinal metastasis from renal cell carcinoma. J Neurosurg Spine 2014;20(1):108-16.
Luksanapruksa P, Buchowski JM, Hotchkiss W, Tongsai S, Wilartratsami S, Chotivichit A. Prognostic factors in patients with spinal metastasis: a systematic review and meta-analysis. Spine J 2017;17(5):689-708.
Paholpak P, Sirichativapee W, Wisanuyotin T, Kosuwon W, Jeeravipoolvarn P. Prevalence of known and unknown primary tumor sites in spinal metastasis patients. Open Orthop J 2012;6:440-4.
Wanman J, Grabowski P, Nystrom H, Gustafsson P, Bergh A, Widmark A, et al. Metastatic spinal cord compression as the first sign of malignancy. Acta Orthop 2017;88(4):457-62.
Aizenberg MR, Fox BD, Suki D, McCutcheon IE, Rao G, Rhines LD. Surgical management of unknown primary tumors metastatic to the spine. J Neurosurg Spine 2012;16(1):86-92.
Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ, Wu Y-L, et al. Lung cancer: current therapies and new targeted treatments. Lancet 2017;389(10066):299-311.
Teo MY, Rathkopf DE, Kantoff P. Treatment of Advanced Prostate Cancer. Annu Rev Med 2019; 70: 479-99.
Sartor O, de Bono JS. Metastatic Prostate Cancer. N Engl J Med 2018;378(7):645-57.
Bakar D, Tanenbaum JE, Phan K, Alentado VJ, Steinmetz MP, Benzel EC, et al. Decompression surgery for spinal metastases: a systematic review. Neurosurg Focus 2016;41(2):E2.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.










