Factors Influencing Willingness to Pay for Teledermatology among Patients with Psoriasis
DOI:
https://doi.org/10.33192/Smj.2022.86Keywords:
Psoriasis, Teledermatology, Telemedicine, Willingness to payAbstract
Objective: To determine the proportion of patients with psoriasis prepared to pay for TD. Attitudes and factors influencing their willingness to pay (WTP) were evaluated.
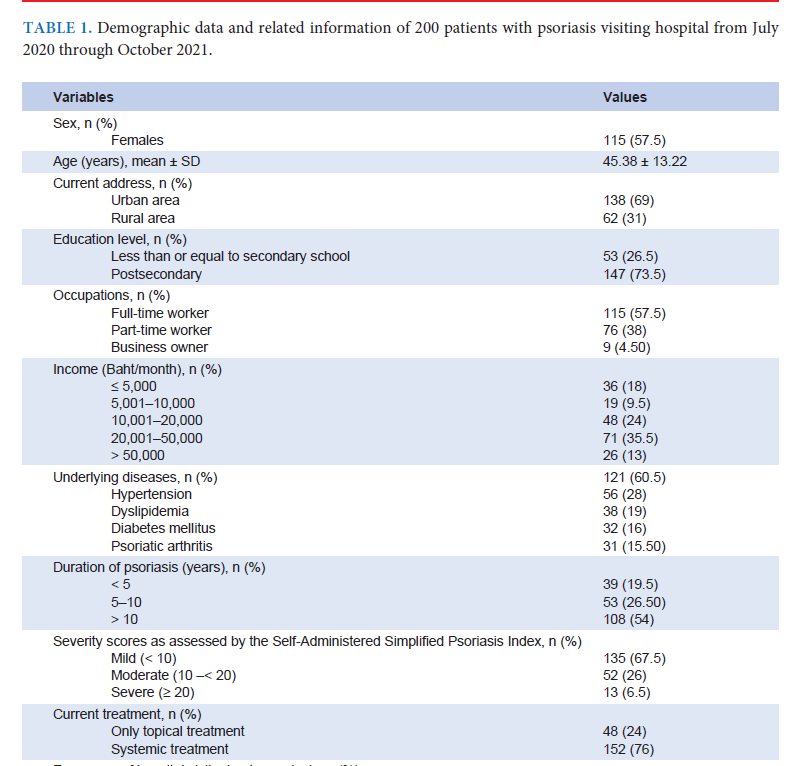
Materials and Methods: This cross-sectional study was conducted from July 2020 to October 2021. Adult patients with psoriasis completed a 2-page self-administered questionnaire.
Results: Of 200 patients, 133 (66.5%) were unfamiliar with TD. However, 144 (72%) were prepared to pay for TD if it were introduced. The majority of patients answered that 300 Bath was the maximum price that they were willing to pay for TD service. Compared with traditional in-person visits, the significant positive influencing factors on WTP were TD’s quicker delivery of treatment, lower costs, and non-inferiority to usual care. Multivariate analysis showed that the independent factors for WTP were higher educational levels, elimination of out-of-pocket, in-hospital visit expenses, owning a business, TD options suited to psoriasis, and no adverse effects on the patient-doctor relationship.
Conclusion: Knowing patients’ attitudes toward TD and the factors influencing their WTP is essential for developing efficient services. Data from this study can be used to develop successful TD services for patients with psoriasis.
References
Pezzolo E, Naldi L. Epidemiology of major chronic inflammatory immune-related skin diseases in 2019. Expert Rev Clin Immunol. 2020;16(2):155-66.
Icen M, Crowson CS, McEvoy MT, Dann FJ, Gabriel SE, Kremes HM. Trends in incidence of adult-onset psoriasis over three decades: a population-based study. J Am Acad Dermatol. 2009;60(3):394-401.
Michalek I, Loring B, John S. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31(2):205-12.
Landow SM, Mateus A, Korgavkar K, Nightingale D, Weinstock MA. Teledermatology: key factors associated with reducing face-to-face dermatology visits. J Am Acad Dermatol. 2014;71(3):570-6.
Elsner P. Teledermatology in the times of COVID‐19–a systematic review. J Dtsch Dermatol Ges. 2020;18(8):841-5.
Coates SJ, Kvedar J, Granstein RD. Teledermatology: from historical perspective to emerging techniques of the modern era: part I: history, rationale, and current practice. J Am Acad Dermatol. 2015;72(4):563-74.
Pasquali P, Sonthalia S, Moreno-Ramirez D, Sharma P, Agrawa M, Gupta S, et al. Teledermatology and its current perspective. Indian Dermatol Online J. 2020;11(1):12-20.
Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of teledermatology on access to dermatology care among Medicaid enrollees. JAMA Dermatol. 2016;152(8):905-12.
Chambers CJ, Parsi KK, Schupp C, Armstrong AW. Patientcentered online management of psoriasis: a randomized controlled equivalency trial. J Am Acad Dermatol. 2012;66(6):948-53.
Wang RH, Barbieri JS, Nguyen HP, Stavert R, Forman HP, Bolognia JL, et al. Clinical effectiveness and cost-effectiveness of teledermatology: Where are we now, and what are the barriers to adoption? J Am Acad Dermatol. 2020;83(1):299-307.
Zakaria A, Maurer T, Su G, Amerson E. Impact of teledermatology on the accessibility and efficiency of dermatology care in an urban safety-net hospital: A pre-post analysis. J Am Acad Dermatol. 2019;81(6):1446-52.
Warshaw EM, Hillman YJ, Greer NL, Hagel EM, MacDonald R, Rutks IR, et al. Teledermatology for diagnosis and management of skin conditions: a systematic review. J Am Acad Dermatol. 2011;64(4):759-72.
Werner P, Karnieli E. A model of the willingness to use telemedicine for routine and specialized care. J Telemed Telecare. 2003;9(5):264-72.
Chularojanamontri L, Wongpraparut C, Winayanuwattikun W, Griffiths CE, Chalmers RJ, et al. A reevaluation of the Simplified Psoriasis Index (SPI) using the Thai language version: a study examining the validity, reliability, and interpretability of SPI when used in translation. Journal of Psoriasis and Psoriatic Arthritis. 2020;5:32-9. Available from: https://doi.org/10.1177/2475530319892196
Dahy A, El‐Qushayri AE, Mahmoud AR, Al-kelany TA, Salman S. Telemedicine approach for psoriasis management, time for application? A systematic review of published studies. Dermatol Ther. 2020;33(6):e13908.
Pearlman RL, Le PB, Brodell RT, Nahar VK. Evaluation of patient attitudes towards the technical experience of synchronous teledermatology in the era of COVID-19. Arch Dermatol Res. 2021;313(9):769-72.
Yeroushalmi S, Millan SH, Nelson K, Sparks A, Friedman AJ. Patient Perceptions and Satisfaction With Teledermatology During the COVID-19 Pandemic: A Survey-Based Study. J Drugs Dermatol. 2021;20(2):178-83.
Qureshi AA, Brandling-Bennett HA, Wittenberg E, Chen SC, Sober AJ, Kvedar JC. Willingness-to-pay stated preferences for telemedicine versus in-person visits in patients with a history of psoriasis or melanoma. Telemed J E Health. 2006;12(6):639-43.
Spinks J, Janda M, Soyer HP, Whitty JA. Consumer preferences for teledermoscopy screening to detect melanoma early. J Telemed Telecare. 2016;22(1):39-46.
Pathipati AS, Ko JM. Implementation and evaluation of Stanford Health Care direct-care teledermatology program. SAGE Open Med. 2016;4:2050312116659089.
Mori WS, Houston N, Moreau JF, Prevost N, Gehris RP, Ferris LK, et al. Personal burden of isotretinoin therapy and willingness to pay for electronic follow-up visits. JAMA Dermatol. 2016;152(3):338-40.
Snoswell CL, Whitty JA, Caffery LJ, Loescher LJ, Gillespie N, Janda M. Direct-to-consumer mobile teledermoscopy for skin cancer screening: Preliminary results demonstrating willingness to pay in Australia. J Telemed Telecare. 2018;24(10):683-9.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














