Long-term Oncologic Outcomes After Curative Surgery in Stage I–III Thai Colorectal Cancer Patients
DOI:
https://doi.org/10.33192/Smj.2022.87Keywords:
Colorectal cancer, long-term outcomes, overall survival, disease-free survival, Asian, ThaiAbstract
Objective: The survival rate for colorectal cancer varies and there are limited reports regarding the long-term outcomes after curative treatment in Thai patients. This study aimed to determine the long-term oncologic results in non-metastatic Thai colorectal cancer patients after curative surgery.
Materials and Methods: We performed a retrospective review of a prospectively collected colorectal cancer registry. Short-term and long-term outcomes were analyzed.
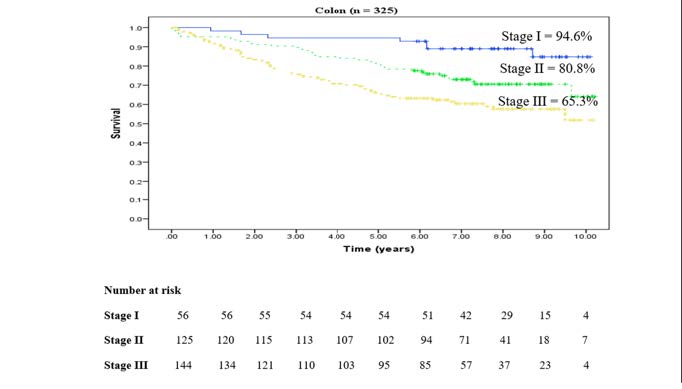
Results: Six hundred and sixty two patients were included in the study, 51.9% colon cancer and 48.1% rectal cancer patients. The mean age was 63.6 ± 12.7 years. The median follow-up time was 5.4 years [IQR: 2.1–7.4]. The 5-year local recurrence was 6.4%; 3.3% in colon cancer and 9.9% in rectal cancer. The 5-year overall survival (5-yr OS) in the colon cancer patients was 76.3%; 94.6% in stage I, 80.8% in stage II, and 65.3% in stage III. The 5-yr OS in the rectal cancer patients was 65.1%; 84.7% in stage I, 75% in stage II, and 51% in stage III. The 5-year disease-free survival (5-yr DFS) in the colon cancer patients was 76.5%; 91.4% in stage I, 81.3% in stage II, and 66.4% in stage III. The 5-yr DFS in the rectal cancer patients was 63.8%; 81.5% in stage I, 75.1% in stage II, and 50.1% in stage III.
Conclusion: The long-term oncologic outcomes after curative treatments in this study were acceptable. The prognosis of treatment depends on the disease stage. Comparing stage by stage, colon cancer has a better prognosis than rectal cancer.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5): E359-86.
Brenner H, Hoffmeister M, Arndt V, Haug U. Gender differences in colorectal cancer: implications for age at initiation of screening. Br J Cancer. 2007;96(5):828-31.
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-64.
Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89-103.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66(4):683-91.
Abancens M, Bustos V, Harvey H, McBryan J, Harvey BJ. Sexual Dimorphism in Colon Cancer. Front Oncol. 2020;10:607909.
Gao RN, Neutel CI, Wai E. Gender differences in colorectal cancer incidence, mortality, hospitalizations and surgical procedures in Canada. J Public Health (Oxf). 2008;30(2):194-201.
Tilney HS, Heriot AG, Purkayastha S, Antoniou A, Aylin P, Darzi AW, et al. A national perspective on the decline of abdominoperineal resection for rectal cancer. Ann Surg. 2008;247(1):77-84.
Keller DS, Reif de Paula T, Kiran RP. Ready for the National Accreditation Programs for Rectal Cancer? Auditing rectal cancer outcomes in the United States. Colorectal Dis. 2019;21(10):1213-5.
Roxburgh CSD, Strombom P, Lynn P, Cercek A, Gonen M, Smith JJ, et al. Changes in the multidisciplinary management of rectal cancer from 2009 to 2015 and associated improvements in short-term outcomes. Colorectal Dis. 2019;21(10):1140-50.
Warschkow R, Ebinger SM, Brunner W, Schmied BM, Marti L. Survival after Abdominoperineal and Sphincter-Preserving Resection in Nonmetastatic Rectal Cancer: A Population-Based Time-Trend and Propensity Score-Matched SEER Analysis. Gastroenterol Res Pract. 2017;2017:6058907.
Marwan K, Staples MP, Thursfield V, Bell SW. The rate of abdominoperineal resections for rectal cancer in the state of Victoria, Australia: a population-based study. Dis Colon Rectum. 2010;53(12):1645-51.
Obias VJ, Reynolds HL Jr. Multidisciplinary teams in the management of rectal cancer. Clin Colon Rectal Surg. 2007;20(3):143-7.
Peng D, Cheng YX, Cheng Y. Improved Overall Survival of Colorectal Cancer under Multidisciplinary Team: A Meta-Analysis. Biomed Res Int. 2021;2021:5541613.
Fehervari M, Hamrang-Yousefi S, Fadel MG, Mills SC, Warren OJ, Tekkis PP, et al. A systematic review of colorectal multidisciplinary team meetings: an international comparison. BJS Open. 2021;5(3):zrab044.
Bhoday J, Martling A, Straßburg J, Brown G. Session 1: The surgeon as a prognostic factor in colon and rectal cancer?. Colorectal Dis. 2018;20 Suppl 1:36-38.
Hermanek P, Mansmann U, Staimmer DS, Riedl S, Hermanek P. The German experience: the surgeon as a prognostic factor in colon and rectal cancer surgery. Surg Oncol Clin N Am. 2000;9(1):33-49, vi.
Porter GA, Soskolne CL, Yakimets WW, Newman SC. Surgeonrelated factors and outcome in rectal cancer. Ann Surg. 1998;227(2):157-67.
van Gijn W, Gooiker GA, Wouters MW, Post PN, Tollenaar RA, van de Velde CJ. Volume and outcome in colorectal cancer surgery. Eur J Surg Oncol. 2010;36 Suppl 1:S55-63.
van Groningen JT, Marang-van de Mheen PJ, Henneman D, Beets GL, Wouters MWJM. Surgeon perceived most important factors to achieve the best hospital performance on colorectal cancer surgery: a Dutch modified Delphi method. BMJ Open. 2019;9(9):e025304.
Renzulli P, Lowy A, Maibach R, Egeli RA, Metzger U, Laffer UT. The influence of the surgeon’s and the hospital’s caseload on survival and local recurrence after colorectal cancer surgery. Surgery. 2006;139(3):296-304.
Techawathanawanna S, Nimmannit A, Akewanlop C. Clinical characteristics and disease outcome of UICC stages I-III colorectal cancer patients at Siriraj Hospital. J Med Assoc Thai. 2012;95 Suppl 2:S189-98.
Yuan Y, Li MD, Hu HG, Dong CX, Chen JQ, Li XF, et al. Prognostic and survival analysis of 837 Chinese colorectal cancer patients. World J Gastroenterol. 2013; 19(17):2650-9.
O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004; 96(19):1420-5.
Liang J, Fazio V, Lavery I, Remzi F, Hull T, Strong S, et al. Primacy of surgery for colorectal cancer. Br J Surg. 2015;102(7):847-52.
Sargent DJ, Wieand HS, Haller DG, Gray R, Benedetti JK, Buyse M, et al. Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2005;23(34):8664-70.
Foxtrot Collaborative Group. Feasibility of preoperative chemotherapy for locally advanced, operable colon cancer: the pilot phase of a randomized controlled trial. Lancet Oncol. 2012;13(11):1152-60.
Schrag D, Weiser MR, Goodman KA, Gonen M, Hollywood E, Cercek A, et al. Neoadjuvant chemotherapy without the routine use of radiation therapy for patients with locally advanced rectal cancer: a pilot trial. J Clin Oncol. 2014;32(6):513-8.
Garcia-Aguilar J, Chow OS, Smith DD, Marcet JE, Cataldo PA, Varma MG, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16(8):957-66.
Bahadoer RR, Dijkstra EA, van Etten B, Marijnen CAM, Putter H, Kranenbarg EM, et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(1):29-42.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














