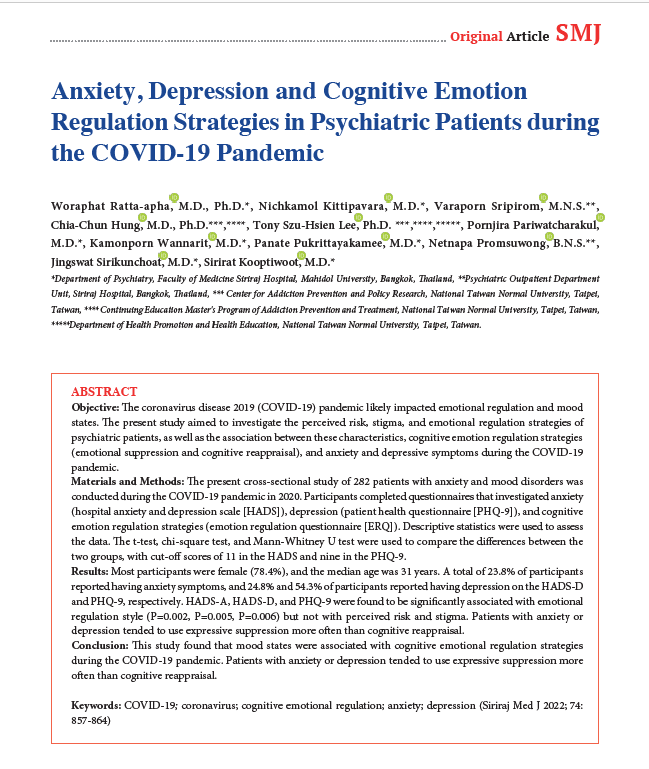
Anxiety, Depression and Cognitive Emotion Regulation Strategies in Psychiatric Patients during the COVID-19 Pandemic
DOI:
https://doi.org/10.33192/Smj.2022.100Keywords:
COVID-19, coronavirus, cognitive emotional regulation, anxiety, depressionAbstract
Objective: The coronavirus disease 2019 (COVID-19) pandemic likely impacted emotional regulation and mood states. The present study aimed to investigate the perceived risk, stigma, and emotional regulation strategies of psychiatric patients, as well as the association between these characteristics, cognitive emotion regulation strategies (emotional suppression and cognitive reappraisal), and anxiety and depressive symptoms during the COVID-19 pandemic.
Materials and Methods: The present cross-sectional study of 282 patients with anxiety and mood disorders was conducted during the COVID-19 pandemic in 2020. Participants completed questionnaires that investigated anxiety (hospital anxiety and depression scale [HADS]), depression (patient health questionnaire [PHQ-9]), and cognitive emotion regulation strategies (emotion regulation questionnaire [ERQ]). Descriptive statistics were used to assess the data. The t-test, chi-square test, and Mann-Whitney U test were used to compare the differences between the two groups, with cut-off scores of 11 in the HADS and nine in the PHQ-9.
Results: Most participants were female (78.4%), and the median age was 31 years. A total of 23.8% of participants reported having anxiety symptoms, and 24.8% and 54.3% of participants reported having depression on the HADS-D and PHQ-9, respectively. HADS-A, HADS-D, and PHQ-9 were found to be significantly associated with emotional regulation style (P=0.002, P=0.005, P=0.006) but not with perceived risk and stigma. Patients with anxiety or depression tended to use expressive suppression more often than cognitive reappraisal.
Conclusion: This study found that mood states were associated with cognitive emotional regulation strategies during the COVID-19 pandemic. Patients with anxiety or depression tended to use expressive suppression more often than cognitive reappraisal.
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
World Health Organization [Internet]. 2020 [cited 2022 Apr 1]. Available from: https://www.who.int/director-general/speeches/detail/
Dechsupa S, Assawakosri S, Phakham S, Honsawek S. Positive impact of lockdown on COVID-19 outbreak in Thailand. Travel Med Infect Dis. 2020;36:101802.
Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300-2.
Das S, Padhy RN, Pradhan BB. A Scenario of COVID-19 Disease on Mental Health Among the General Age-groups. Siriraj Med J. 2022;74:64-7.
Simon J, Helter TM, White RG, van der Boor C, Łaszewska A. Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: an Austrian survey study. BMC Public Health. 2021;21:314.
Pulla P. Covid-19: India imposes lockdown for 21 days and cases rise. BMJ. 2020; 368:m1251.
Poyraz BÇ, Poyraz CA, Olgun Y, Gürel Ö, Alkan S, Özdemir YE, et al. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry Res. 2021;295:113604.
Maneepongpermpoon P, Pitanupong J. Knowledge, Risk Perception, Precautionary Behavior and Level of Worry towards the 2019 Coronavirus Disease (COVID-19) among Psychiatric Outpatients. Siriraj Med J. 2020;73:1-9.
Gross JJ. The Emerging Field of Emotion Regulation: An Integrative Review. Publ. Found. 1998;2:271-99.
Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348-62.
Tyra AT, Griffin SM, Fergus TA, Ginty AT. Individual differences in emotion regulation prospectively predict early COVID-19 related acute stress. J Anxiety Disord. 2021;81:102411.
Schudy A, Żurek K, Wiśniewska M, Piejka A, Gawęda Ł, Okruszek Ł. Mental Well-Being During Pandemic: The Role of Cognitive Biases and Emotion Regulation Strategies in Risk Perception and Affective Response to COVID-19. Front Psychiatry. 2020;11:589973.
Low RST, Overall NC, Chang VT, Henderson AME, Sibley CG. Emotion regulation and psychological and physical health during a nationwide COVID-19 lockdown. Emotion. 2021;21(8):1671-90.
Pérez S, Masegoso A, Hernández-Espeso N. Levels and variables associated with psychological distress during confinement due to the coronavirus pandemic in a community sample of Spanish adults. Clin Psychol Psychother. 2021;28:606-14.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13.
Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8:46.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-70.
Nilchaikobit T, Lortrakul M, Phisansuthideth U. Development of Thai version of hospital anxiety and depression scale in cancer patients. J Psychiatr Assoc Thailand. 1996;41:18-30.
Khumrod N, Soonthornchaiya R. The effect of the emotion regulation program on depressive symptoms among patients with major depressive disorder. The Journal of Psychiatric Nursing and Mental Health. 2017;31:136-50.
Koole SL. The psychology of emotion regulation: An integrative review. Cognition and Emotion. 2009;23(1):4-41.
John OP, Gross JJ. Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J Pers. 2004;72:1301-33.
Hu T, Zhang D, Wang J, Mistry R, Ran G, Wang X. Relation between emotion regulation and mental health: a meta-analysis review. Psychol Rep. 2014;114:341-62.
Cardi V, Albano G, Gentili C, Sudulich L. The impact of emotion regulation and mental health difficulties on health behaviours during COVID19. J Psychiatr Res. 2021;143:409-15.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














