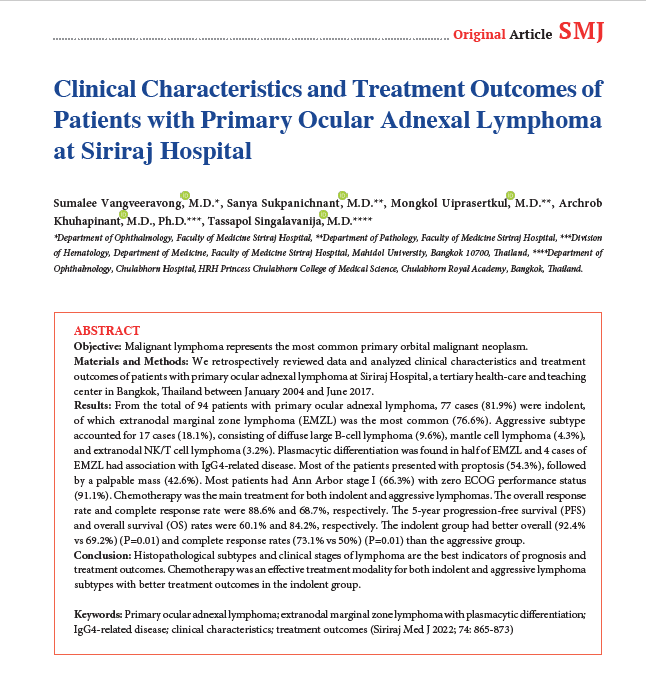
Clinical Characteristics and Treatment Outcomes of Patients with Primary Ocular Adnexal Lymphoma at Siriraj Hospital
DOI:
https://doi.org/10.33192/Smj.2022.101Keywords:
Primary ocular adnexal lymphoma, extranodal marginal zone lymphoma with plasmacytic differentiation, IgG4-related disease, clinical characteristics, treatment outcomesAbstract
Objective: Malignant lymphoma represents the most common primary orbital malignant neoplasm.
Materials and Methods: We retrospectively reviewed data and analyzed clinical characteristics and treatment outcomes of patients with primary ocular adnexal lymphoma at Siriraj Hospital, a tertiary health-care and teaching center in Bangkok, Thailand between January 2004 and June 2017.
Results: From the total of 94 patients with primary ocular adnexal lymphoma, 77 cases (81.9%) were indolent, of which extranodal marginal zone lymphoma (EMZL) was the most common (76.6%). Aggressive subtype accounted for 17 cases (18.1%), consisting of diffuse large B-cell lymphoma (9.6%), mantle cell lymphoma (4.3%), and extranodal NK/T cell lymphoma (3.2%). Plasmacytic differentiation was found in half of EMZL and 4 cases of EMZL had association with IgG4-related disease. Most of the patients presented with proptosis (54.3%), followed by a palpable mass (42.6%). Most patients had Ann Arbor stage I (66.3%) with zero ECOG performance status (91.1%). Chemotherapy was the main treatment for both indolent and aggressive lymphomas. The overall response rate and complete response rate were 88.6% and 68.7%, respectively. The 5-year progression-free survival (PFS) and overall survival (OS) rates were 60.1% and 84.2%, respectively. The indolent group had better overall (92.4% vs 69.2%) (P=0.01) and complete response rates (73.1% vs 50%) (P=0.01) than the aggressive group.
Conclusion: Histopathological subtypes and clinical stages of lymphoma are the best indicators of prognosis and treatment outcomes. Chemotherapy was an effective treatment modality for both indolent and aggressive lymphoma subtypes with better treatment outcomes in the indolent group.
References
Fung CY, Tarbell NJ, Lucarelli MJ, Goldberg SI, Linggood RM, Harris NL, et al. Ocular adnexal lymphoma: clinical behavior of distinct World Health Organization classification subtypes. Int J Radial Oncol Biol Phys. 2003;57:1382-91.
Sasai K, Yamabe H, Dodo Y, Kashii S, Nagata Y, Hiraoka M. Non-Hodgkin’s lymphoma of the ocular adnexa. Acta Oncol. 2001;40:485-90.
Bayraktar S. Bayraktar UD, Stefanovic A, Lossos IS. Primary ocular adnexal mucosa-associated lymphoid tissue lymphoma (MALT): single institution experience in a large cohort of patients. Br J Haematol. 2011;152:72-80.
White WL, Ferry JA, Harris NL, Grove AS Jr. Ocular adnexal lymphoma: a clinicopathologic study with identification of lymphomas of mucosa-associated lymphoid tissue type. Ophthalmology. 1995;102:1994-2006.
McKelvie PA, McNab A, Francis IC, Fox R, O’Day J. Ocular adnexal lymphoproliferative disease: a series of 73 cases. Clin Experiment Ophthalmol. 2001;29:387-93.
Coupland SE, Krause L, Delecluse HJ, Anagnostopoulos I, Foss HD, Hummel M, et al. Lymphoproliferative lesions of the ocular adnexa: analysis of 112 cases. Ophthalmology. 1998;105:1430-41.
Jenkins C, Rose GE, Bunce C, Wright JE, Cree IA, Plowman N, et al. Histological features of ocular adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Br J Ophthalmol. 2000;84:907-13.
Ferry JA, Fung CY, Zukerberg L, Lucarelli MJ, Hasserjian RP, Preffer FI,net al. Lymphoma of the ocular adnexa: a study of 353 cases. Am J Surg Pathol. 2007;31:170-84.
Cho EY, Han JJ, Ree HJ, Ko YH, Kang YK, Ahn HS, et al. Clinicopathologic analysis of ocular adnexal lymphomas: extranodal marginal zone B-cell lymphoma constitutes the vast majority of ocular lymphomas among Koreans and affects younger patients. Am J Hematol. 2003;73:87-96.
Sullivan TJ, Whitehead K, Williamson R, Grimes D, Schlect D, Brown I, et al. Lymphoproliferative disease of the ocular adnexa: a clinical and pathologic study with statistical analysis of 69 patients. Ophthal Plast Reconstr Surg. 2005;21:177-88.
Sullivan TJ, Valenzuela AA. Imaging features of ocular adnexal lymphoproliferative disease. Eye (Lond). 2006;20:1189-95.
Yen MT, Bilyk JR, Wladis EJ, Bradley EF, Mawn LA. Treatments for ocular adnexal lymphoma A report by the American Academy of Ophthalmology. Ophthalmology. 2018;125:127-36.
Seresirikachorn S, Ausayakhun S, Wiwatwongwana D, Maha nupab P, Daroontum T, Norasetthada L. Characteristics and treatment outcomes of patients with primary ocular adnexal lymphoma in Northern Thailand. Asian J Ophthalmol.2020;17:86-97.
Swerdlow SH, Kuzu I, Dogan A, Dirnhofer S, Chan JK, Sander B, et al. The many faces of small B cell lymphomas with plasmacytic differentiation and the contribution of MYD88 testing. Virchows Arch. 2016;468:259-75.
Cheuk W, Yuen HK, Chan AC, Shih LY, Kuo TT, Ma MW, et al. Ocular adnexal lymphoma associated with IgG4+ chronic sclerosing dacryoadenitis: a previously undescribed complication of IgG4-related sclerosing disease. Am J Surg Pathol. 2008;32:1159-67.
Ohno K, Sato Y, Ohshima K, Takata K, Takata TM, Gion Y, et al. A subset of ocular adnexal marginal zone lymphomas may arise in association with IgG4-related disease. Sci Rep. 2015;5:13539.
Rootman DB, Mavrikakis I, Connors JM, Rootman J. Primary, unilateral ocular adnexal lymphoma: disease progression and long-term survival. Ophthal Plast Reconstr Surg. 2011;27:405-9.
Rosado MF, Byrne Jr GE, Ding F, Fields KA, Ruiz P, Dubovy SR, et al. Ocular adnexal lymphoma: a clinicopathologic study of a large cohort of patients with no evidence for an association with Chlamydia psittaci. Blood. 2006;107:467-72.
Tanimoto K, Kaneko A, Suzuki S, Sekiguchi N, Watanabe T, Kobatashi Y, et al. Primary ocular adnexal MALT lymphoma: a long-term follow-up study of 114 patients. Jpn J Clin Oncol. 2007;37:337-44.
De Cicco L, Cella L, Liuzzi R, Solla R, Farella A, Punzo G, et al. Radiation therapy in primary orbital lymphoma: a single institution retrospective analysis. Radiat Oncol. 2009;4:60.
Yoon JS, Ma KT, Kim SJ, Kook K, Lee SY. Prognosis for patients in a Korean population with ocular adnexal lymphoproliferative lesions. Ophthal Plast Reconstr Surg. 2007;23:94-99.
Jenkins C, Rose GE, Bunce C, Wright JE, Cree IA, Plowman N, et al. Histological features of ocular adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Br J Ophthalmol. 2000;84:907-13.
Coupland SE, Hellmich M, Auw-Haedrich C, Lee WR, Anagnostopoulos I, Stein H. Plasmacellular differentiation in extranodal marginal zone B cell lymphomas of the ocular adnexa: an analysis of the neoplastic plasma cell phenotype and its prognostic significance in 136 cases. Br J Ophthalmol. 2005;89:352-9.
Meunier J, Lumbroso-Le RL, Vincent-Salomon A, Dendale R, Asselain B, Arnaud P, et al. Ophthalmologic and intraocular non-Hodgkin’s lymphoma: a large single center study of initial characteristics, natural history, and prognostic factors. Hematol Oncol. 2004;22:143-58.
Konig L, Stade R, Rieber J, Debus J, Herfarth K. Radiotherapy of indolent orbital lymphomas: two radiation concepts. Strahlenther Onkol. 2016;192:414-21.
Woolf DK, Kuhan H, Shoffren O, Akinnawo, EM, Sivagurunathan B, Boyce H, et al. Outcomes of primary lymphoma of the ocular adnexa (orbital lymphoma) treated with radiotherapy. Clin Oncol (R Coll Radiol). 2015;27:153-9.
Ferry JA, Fung CY, Zukerberg L, Lucarelli MJ, Hasserjian RP, Preffer FI, et al. Lymphoma of the ocular adnexa: a study of 353 cases. Am J Surg Pathol. 2007;31:170-84.
Portell CA, Aronow ME, Rybicki LA, Macklis R, Singh AD, Sweetenham JW. Clinical characteristics of 95 patients with ocular adnexal and uveal lymphoma: treatment Outcomes in Extranodal Marginal Zone Subtype. Clin Lymphoma Myeloma Leuk. 2014;14(3):203-10.
Sniegowski MC, Robert D, Bakhoum M, Laughlin PM, Yin VT, Turturro F, et al. Ocular adnexal lymphoma: validation of American Joint Committee on Cancer seventh edition staging guidelines. Br J Ophthalmol. 2014;98:1255-60.
Parikh RR, Moskowitz BK, Maher E, Rocca DD, Rocca RB, Culliney B, et al. Long-term outcomes and patterns of failure in orbital lymphoma treated with primary radiotherapy. Leuk Lymphoma. 2015;56:1266-70.
Stafford SL, Kozelsky TF, Garrity JA, Kurtin PJ, Leavitt JA, Martenson JA, et al. Orbital lymphoma: radiotherapy outcome and complications. Radiother Oncol. 2001;59:139-44.
Yadav BS, Sharma SC. Orbital lymphoma: role of radiation. Indian J Ophthalmol 2009;57(2): 91-7.
Watkins LM, Carter KD, Nerad JA. Ocular adnexal lymphoma of the extraocular muscles: case series from the University of Iowa and review of the literature. Ophthal Plast Reconstr Surg 2011;27:471-6.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














