Peripheral Atherosclerotic Profile in Type 1 Diabetic Patients: Lipid Ratios as a Predictive Marker of Asymptomatic Patients
DOI:
https://doi.org/10.33192/Smj.2022.102Keywords:
Ankle-brachial index, asymptomatic peripheral artery disease, atherosclerosis, lipid ratiosAbstract
Objective: To investigate the relationship between Lipid ratios and asymptomatic peripheral artery disease (aPAD) in type 1 diabetic patients.
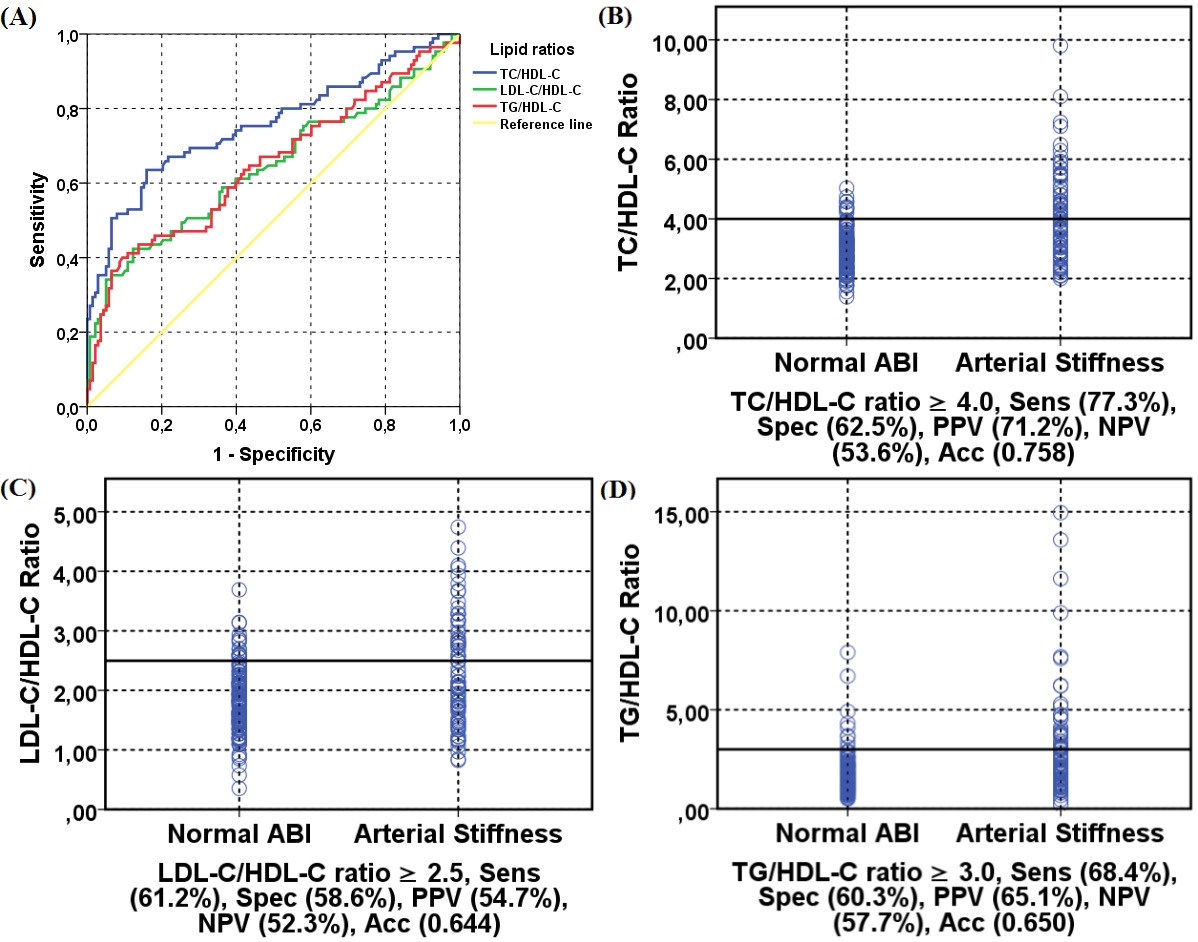
Materials and Methods: This cross-sectional study was performed among 223 diabetics. Patients were segregated with aPAD when their ankle-brachial index (ABI) was abnormal (ABI ≤ 0.90, or ABI > 1.20). Patients were segregated into the following groups (patients with normal ABI vs. patients with arterial stiffness). The association between lipid ratios and aPAD was analyzed using multivariate logistic regression analysis and the receiver operator characteristic curve.
Results: Our study reported a slight preponderance of females (108 males vs. 115 females), with a mean age of 30.70±9.69 years and a diabetes duration of 11.13±8.95 years. The prevalence of arterial stiffness was 38.11%. TC/HDL-C ratio was a significant predictor for atherosclerosis with a sensitivity of 77.3%, specificity of 62.5%, and diagnostic accuracy of 0.758%. The results revealed that the 4th quartile (odds ratio [OR]=12.52 [5.06-31.00], p=<0.001) of TC/HDL-C ratio was statistically higher in patients with arterial stiffness. Similarly, the last quartiles of LDL-C/HDL-C and TG/HDL-C ratio were higher in the arterial stiffness group (OR=3.70 [1.68-8.11], p=0.001; OR=4.74 [2.12-10.59], p=<0.001; respectively). In the arterial stiffness group, non-traditional lipid values were significantly higher in males compared to females.
Conclusion: Lipid ratios are correlated with aPAD in type 1 diabetic patients, and should thus be assessed in clinical decision-making and risk stratification on atherosclerotic cardiovascular disease.
References
de Ferranti SD, de Boer IH, Fonseca V, Fox CS, Golden SH, Lavie CJ, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Circulation 2014;130:1110-30.
Hinchliffe RJ, Brownrigg JR, Apelqvist J, Boyko EJ, Fitridge R, Mills JL, et al. IWGDF guidance on the diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes. Diabetes Metab Res Rev 2016;32:37-44.
Crawford F, Welch K, Andras A, Chappell FM. Ankle brachial index for the diagnosis of lower limb peripheral arterial disease. Cochrane Database Syst Rev 2016;9:CD010680.
Sobhani S, Asayesh H, Sharifi F, Djalalinia S, Baradaran HR, Arzaghi SM, et al. Prevalence of diabetic peripheral neuropathy in Iran: a systematic review and metaanalysis. J Diabetes Metab Disord 2014;13:97.
Davies M, Brophy S, Williams R, Taylor A. The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care 2006;29:1518-22.
Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes 2015;6:961-9.
Dua A, Lee CJ. Epidemiology of Peripheral Arterial Disease and Critical Limb Ischemia. Tech Vasc Interv Radiol 2016;19:91-5.
Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries Endorsed by: the European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J 2018;39:763-816.
International Diabetes Federation. IDF Diabetes Atlas, 9th ed. Brussels, 2019.p.88-9.
Elgzyri T, Larsson J, Thorne J, Eriksson KF, Apelqvist J. Outcome of ischemic foot ulcer in diabetic patients who had no invasive vascular intervention. Eur J Vasc Endovasc Surg 2013;46:110-17.
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease. Circulation 2006;113:e463-654.
Urbina EM, Wadwa RP, Davis C, Snively BM, Dolan LM, Daniels SR, et al. Prevalence of increased arterial stiffness in children with type 1 diabetes mellitus differs by measurement site and sex: the SEARCH for Diabetes in Youth Study. J Pediatr. 2010;156:731-7.
Cecelja M, Chowienczyk P. Role of arterial stiffness in cardiovascular disease. JRSM Cardiovasc Dis 2012;1:1-10.
Joosten MM, Pai JK, Bertoia ML, Rimm EB, Spiegelman D, Mittleman MA, et al. Associations between conventional cardiovascular risk factors and risk of peripheral artery disease in men. JAMA 2012;308:1660-7.
Aponte J. The prevalence of asymptomatic and symptomatic peripheral arterial disease and peripheral arterial disease risk factors in the US population. Holist Nurs Pract 2011;25:147-61.
Wongtiraporn W, Luenee P, Opartkiattikul N, Wongtiraporn W, Laiwejpithaya S, Sangkarat S, et al. Tissue Factor Expression of Endothelial Cell in Response to Atherosclerotic Risk Factors. Siriraj Med J 2011;63:1-3.
Su Y, Zhang R, Xu R, Wang H, Geng H, Pan M, et al. Triglyceride to high-density lipoprotein cholesterol ratio as a risk factor of repeat revascularization among patients with acute coronary syndrome after first-time percutaneous coronary intervention. J Thorac Dis 2019;11:5087-95.
Jia L, Long S, Fu M, Yan B, Tian Y, Xu Y, et al. Relationship between total cholesterol/high-density lipoprotein cholesterol ratio, triglyceride/high-density lipoprotein cholesterol ratio, and high-density lipoprotein subclasses. Metabolism 2006;55:1141-8.
Millán J, Pintó X, Muñoz A, Zúñiga M, Rubiés-Prat J, Pallardo LF, et al. Lipoprotein ratios: physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag 2009;5:757-65.
Ridker PM, Stampfer MJ, Rifai N. Novel risk factors for systemic atherosclerosis: a comparison of c-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA 2001;285:2481-5.
Aday AW, Everett BM. Dyslipidemia profiles in patients with peripheral artery disease. Curr Cardiol Rep 2019;21:42.
Zhong Z, Hou J, Zhang Q, Zhong W, Li B, Li C, et al. Assessment of the LDL-C/HDL-C ratio as a predictor of one year clinical outcomes in patients with acute coronary syndromes after percutaneous coronary intervention and drug-eluting stent implantation. Lipids Health Dis 2019;18:40.
American Diabetes Association. 10. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018;41:S105-S18.
Taylor-Piliae RE, Fair JM, Varady AN, Hlatky MA, Norton LC, Iribarren C, et al. Ankle brachial index screening in asymptomatic older adults. Am Heart J 2011;161:979-85.
Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, et al. Measurement and interpretation of the anklebrachial index: a scientific statement from the American Heart Association. Circulation 2012;126:2890-9.
Nattero-Chávez L, Redondo López S, Alonso Díaz S, Garnica Ureña M, Fernández-Durán E, Escobar-Morreale HF, et al. The peripheral atherosclerotic profile in patients with type 1 diabetes warrants a thorough vascular assessment of asymptomatic patients. Diabetes Metab Res Rev 2019;35:e3088.
Nattero-Chávez L, Redondo López S, Alonso Díaz S, Garnica Ureña M, Fernández-Durán E, Escobar-Morreale HF, et al. Association of Cardiovascular Autonomic Dysfunction With Peripheral Arterial Stiffness in Patients With Type 1 Diabetes. J Clin Endocrinol Metab 2019;104:2675-84.
Jude EB, Eleftheriadou I, Tentolouris N. Peripheral arterial disease in diabetes--a review. Diabet Med 2010;27:4-14.
Konin C, Essam N'loo AS, Adoubi A, Coulibaly I, N'guetta R, Boka B, et al. Artériopathie des membres inférieurs du diabétique noir africain: aspects ultrasoniques et facteurs déterminants [Peripheral arterial disease of the lower limbs in African diabetic patients: ultrasonography and determining factors]. J Mal Vasc 2014;39:373-81.
Zander E, Heinke P, Reindel J, Kohnert KD, Kairies U, Braun J, et al. Peripheral arterial disease in diabetes mellitus type 1 and type 2: are there different risk factors? Vasa 2002;31:249-4.
Morley RL, Sharma A, Horsch AD, Hinchliffe RJ. Peripheral artery disease. BMJ 2018;360:j5842.
Adler AI, Stevens RJ, Neil A, Stratton IM, Boulton AJ, Holman RR. UKPDS 59: hyperglycemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 diabetes. Diabetes Care 2002;25:894-9.
Chenglong Z, Jing L, Xia K, Yang T. Association of hemoglobin with ankle-brachial index in general population. Clinics (Sao Paulo) 2016;71:375-80.
Zhao W, Zeng H, Zhang X, Liu F, Pan J, Zhao J, et al. A high thyroid stimulating hormone level is associated with diabetic peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract 2016;115:122-9.
Leening MJ, Ferket BS, Steyerberg EW, Kavousi M, Deckers JW, Nieboer D, et al. Sex differences in lifetime risk and first manifestation of cardiovascular disease: prospective population based cohort study. BMJ 2014;349:g5992.
Madonna R, Balistreri CR, De Rosa S, Muscoli S, Selvaggio S, Selvaggio G, et al. Impact of Sex Differences and Diabetes on Coronary Atherosclerosis and Ischemic Heart Disease. J Clin Med 2019;8:98.
Ness J, Aronow WS, Ahn C. Risk factors for symptomatic peripheral arterial disease in older persons in an academic hospital-based geriatrics practice. J Am Geriatr Soc 2000;48:312-4.
Aday AW, Lawler PR, Cook NR, Ridker PM, Mora S, Pradhan AD. Lipoprotein Particle Profiles, Standard Lipids, and Peripheral Artery Disease Incidence. Circulation 2018;138:2330-41.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














