Recurrent Urinary Tract Infection in Women from a Urologist’s Perspective
DOI:
https://doi.org/10.33192/smj.v75i1.260531Keywords:
Cystitis, urinary tract infection, urologic condition, investigationAbstract
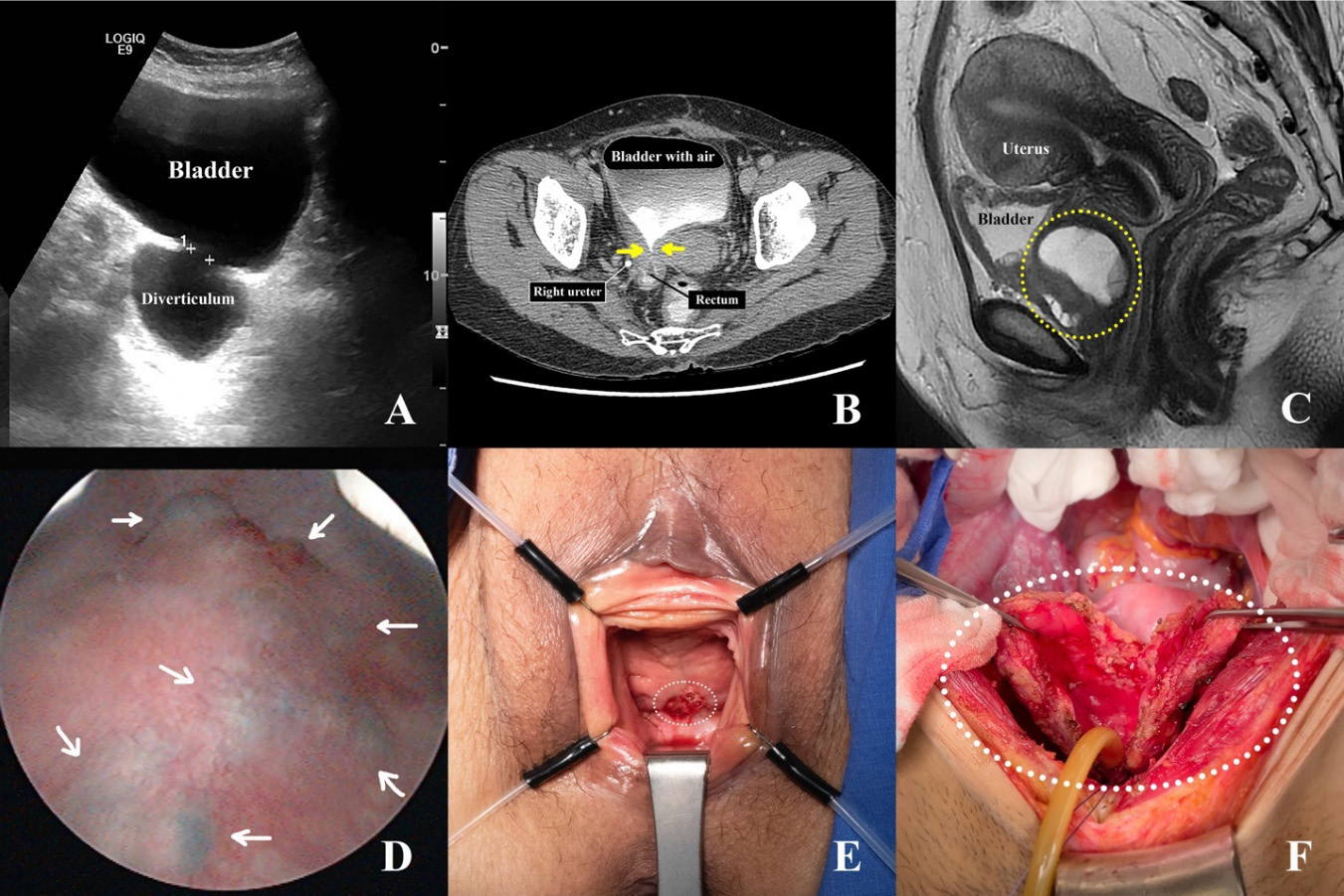
Urinary tract infection (UTI) referred to microbial invasion of the urinary tract system, typically due to bacteria. UTI is more common in women than men, which is thought to be due to differences in lower urinary tract anatomy. Making a diagnosis of UTI begins with the presence of clinical symptoms consistent with either pyelonephritis and cystitis. When pyelonephritis symptoms are present, it is usually associated with bacterial infection, while the symptoms of clinical cystitis may or may not be caused by infection. As both urologic and non-urologic conditions can produce the clinical symptoms of cystitis, diagnosis of UTI requires both pyuria and bacteriuria on urine examination. Complicated UTI is when the infection is associated with either host or bacterial factors that increase the chance of reinfection and decrease treatment efficacy, such as altered organism virulence, immunocompromise, or urinary tract abnormalities. The urologist’s primary role in UTI management is to evaluate for such urinary tract abnormalities and, if needed, resolve those conditions to prevent recurrent infection. This review will describe the urologists’ evaluation and management of complicated and recurrent UTI and inform physician about the urinary tract abnormalities that can predispose to recurrent UTI.
References
Zeng Z, Zhan J, Zhang K, Chen H, Cheng S. Global, regional, and national burden of urinary tract infections from 1990 to 2019: an analysis of the global burden of disease study 2019. World J Urol. 2022;40(3):755-63.
Foxman B, Barlow R, D’Arcy H, Gillespie B, Sobel JD. Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol. 2000;10(8):509-15.
Bent S, Nallamothu BK, Simel DL, Fihn SD, Saint S. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287(20):2701-10.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309-32.
Anger J, Lee U, Ackerman AL, Chou R, Chughtai B, Clemens JQ, et al. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. J Urol. 2019;202(2):282-9.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-20.
Hooton TM, Scholes D, Hughes JP, Winter C, Roberts PL, Stapleton AE, et al. A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med. 1996;335(7):468-74.
Foxman B, Gillespie B, Koopman J, Zhang L, Palin K, Tallman P, et al. Risk factors for second urinary tract infection among college women. Am J Epidemiol. 2000;151(12):1194-205.
Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. Risk factors for recurrent urinary tract infection in young women. J Infect Dis. 2000;182(4):1177-82.
Raz R, Gennesin Y, Wasser J, Stoler Z, Rosenfeld S, Rottensterich E, et al. Recurrent urinary tract infections in postmenopausal women. Clin Infect Dis. 2000;30(1):152-6.
van Haarst EP, van Andel G, Heldeweg EA, Schlatmann TJ, van der Horst HJ. Evaluation of the diagnostic workup in young women referred for recurrent lower urinary tract infections. Urology. 2001;57(6):1068-72.
Santoni N, Ng A, Skews R, Aboumarzouk OM. Recurrent Urinary Tract Infections in Women: What Is the Evidence for Investigating with Flexible Cystoscopy, Imaging and Urodynamics? Urol Int. 2018;101(4):373-81.
Engel G, Schaeffer AJ, Grayhack JT, Wendel EF. The role of excretory urography and cystoscopy in the evaluation and management of women with recurrent urinary tract infection. J Urol. 1980;123(2):190-1.
Fowler JE, Jr., Pulaski ET. Excretory urography, cystography, and cystoscopy in the evaluation of women with urinary-tract infection: a prospective study. N Engl J Med. 1981;304(8):462-5.
Lieberman E, Macchia RJ. Excretory urography in women with urinary tract infection. J Urol. 1982;127(2):263-4.
Aslaksen A, Baerheim A, Hunskaar S, Gothlin JH. Intravenous urography versus ultrasonography in evaluation of women with recurrent urinary tract infection. Scand J Prim Health Care. 1990;8(2):85-9.
Pagano MJ, Barbalat Y, Theofanides MC, Edokpolo L, James MB, Cooper KL. Diagnostic yield of cystoscopy in the evaluation of recurrent urinary tract infection in women. Neurourol Urodyn. 2017;36(3):692-6.
Hijazi S, Leitsmann C. Clinical significance of video-urodynamic in female recurrent urinary tract infections. Int J Womens Health. 2016;8:31-4.
Lee PJ, Kuo HC. High incidence of lower urinary tract dysfunction in women with recurrent urinary tract infections. Low Urine Tract Symptoms. 2020;12(1):33-40.
Albert X, Huertas I, Pereiro, II, Sanfelix J, Gosalbes V, Perrota C. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane Database Syst Rev. 2004(3):CD001209.
Ahmed H, Davies F, Francis N, Farewell D, Butler C, Paranjothy S. Long-term antibiotics for prevention of recurrent urinary tract infection in older adults: systematic review and metaanalysis of randomised trials. BMJ Open. 2017;7(5):e015233.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506-14.
Beerepoot MA, ter Riet G, Nys S, van der Wal WM, de Borgie CA, de Reijke TM, et al. Lactobacilli vs antibiotics to prevent urinary tract infections: a randomized, double-blind, noninferiority trial in postmenopausal women. Arch Intern Med. 2012;172(9):704-12.
Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev. 2015(12):CD008772.
Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008(2):CD005131.
Lee BS, Bhuta T, Simpson JM, Craig JC. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
Harding C, Mossop H, Homer T, Chadwick T, King W, Carnell S, et al. Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women: multicentre, open label, randomised, non-inferiority trial. BMJ. 2022;376:e068229.
Howell AB, Reed JD, Krueger CG, Winterbottom R, Cunningham DG, Leahy M. A-type cranberry proanthocyanidins and uropathogenic bacterial anti-adhesion activity. Phytochemistry. 2005;66(18):2281-91.
Schmidt DR, Sobota AE. An examination of the anti-adherence activity of cranberry juice on urinary and nonurinary bacterial isolates. Microbios. 1988;55(224-225):173-81.
Sobota AE. Inhibition of bacterial adherence by cranberry juice: potential use for the treatment of urinary tract infections. J Urol. 1984;131(5):1013-6.
Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD001321.
Redmond EJ, Murphy CF, Leonard J, Faulds K, Abdelfadil S, Crowley VE, et al. The influence of dietary supplementation with cranberry tablets on the urinary risk factors for nephrolithiasis. World J Urol. 2019;37(3):561-6.
Chughtai B, Thomas D, Howell A. Variability of commercial cranberry dietary supplements for the prevention of uropathogenic bacterial adhesion. Am J Obstet Gynecol. 2016;215(1):122-3.
Howell AB, Dreyfus JF, Chughtai B. Differences in Urinary Bacterial Anti-Adhesion Activity after Intake of Cranberry Dietary Supplements with Soluble versus Insoluble Proanthocyanidins. J Diet Suppl. 2022;19(5):621-39.
Schaeffer AJ, Amundsen SK, Jones JM. Effect of carbohydrates on adherence of Escherichica coli to human urinary tract epithelial cells. Infect Immun. 1980;30(2):531-7.
Aronson M, Medalia O, Schori L, Mirelman D, Sharon N, Ofek I. Prevention of colonization of the urinary tract of mice with Escherichia coli by blocking of bacterial adherence with methyl alpha-D-mannopyranoside. J Infect Dis. 1979;139(3):329-32.
Lenger SM, Bradley MS, Thomas DA, Bertolet MH, Lowder JL, Sutcliffe S. D-mannose vs other agents for recurrent urinary tract infection prevention in adult women: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;223(2):265.e1-265.e13.
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














