Routine Fogarty Catheter Occlusion of Fistula in Esophageal Atresia with Tracheoesophageal Fistula Surgery: A Retrospective Study
DOI:
https://doi.org/10.33192/smj.v75i5.260704Keywords:
congenital esophageal atresia (EA), Fogarty catheter, outcomes, tracheoesophageal fistula (TEF)Abstract
Objective: We aimed to analyze the outcomes of patients who underwent surgical repair of congenital esophageal atresia (EA) with a distal tracheoesophageal fistula (EA/TEF) or a Gross type C with successful routine Fogarty catheter occlusion of TEF.
Materials and Methods: We retrospectively reviewed the medical records of patients who underwent surgical repair of Gross type C with successful routine Fogarty catheter occlusion of fistula between April 2010 and November 2016.
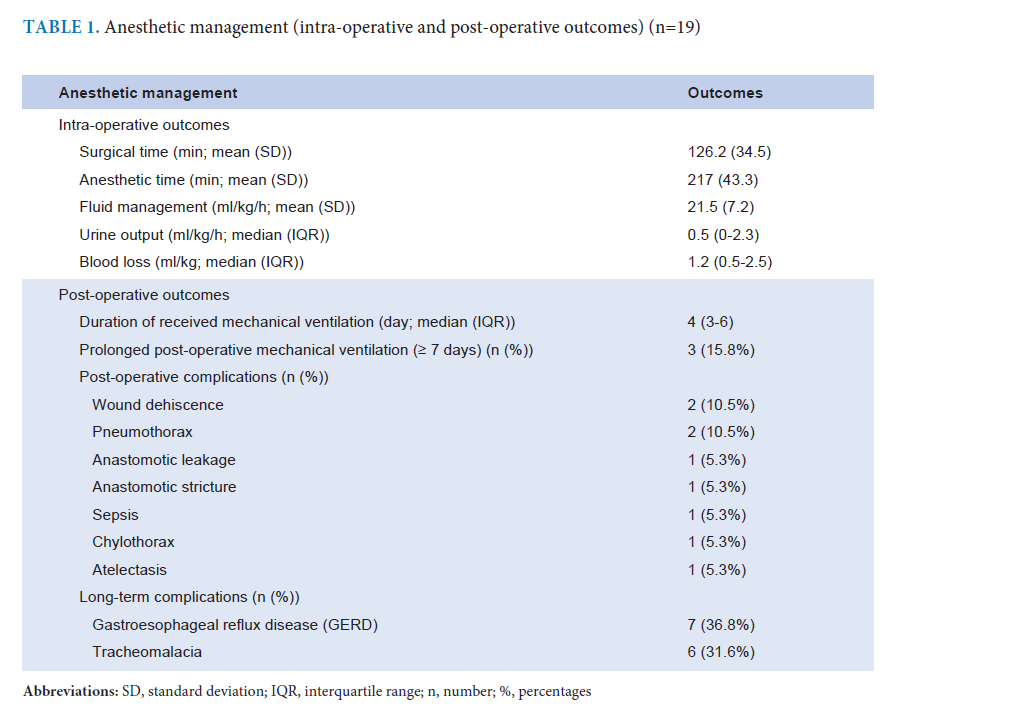
Results: Nineteen patients were enrolled and included for analysis. Mean gestational age was 38.7 (1.9) weeks with 2 (10.5%) neonates born prematurely. Mean birthweight was 2569.3 (425.3) g. Five (26.3%) patients required mechanical ventilation (MV) before surgical repair of TEF. Median post-operative required MV after TEF surgery was 4 (3-6) days. The most common of post-operative complications were wound dehiscence (10.5%) and pneumothorax (10.5%). Long-term complications were gastroesophageal reflux disease (36.8%) and tracheomalacia (31.6%).
Conclusion: The success rate of routine TEF occlusion with a Fogarty catheter was 86.4%. Routine Fogarty catheter occlusion of TEF can be used safely with experienced personnel, low incidence of aspiration and satisfied ventilation. There was no serious complication associated with placement of Fogarty catheter or catheter dislodgement, and it did not occur during any of the procedures.
References
Khan S, Matta SR. Congenital anomalies: Esophageal atresia and tracheoesophageal fistula. In: Kliegman RM, Geme JS, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson textbook of pediatrics. 21th ed. Philadelphia, PA: Elsevier; 2019. p.1929-31.
Uzumcugil F. Anesthetic management of tracheo-esophageal fistula. Curr Chall Thorac Surg. 2022;4:27. doi:10.21037/ccts-20-183
Yang CF, Soong WJ, Jeng MJ, Chen SJ, Lee YS, Tsao PC, et al. Esophageal atresia with tracheoesophageal fistula: ten years of experience in an institute. J Chin Med Assoc. 2006;69(7):317-21. doi:10.1016/S1726-4901(09)70265-5
Knottenbelt G, Costi D, Stephens P, Beringer R, Davidson A. An audit of anesthetic management and complications of tracheo-esophageal fistula and esophageal atresia repair. Paediatr Anaesth. 2012;22(3):268-74. doi:10.1111/j.1460-9592.2011.03738.x
Chang JW, Choo O, Shin YS, Hong J, Kim C. Temporary closure of congenital tracheoesophageal fistula with Fogarty catheter. Laryngoscope. 2013;123(12):3219-22. doi:10.1002/lary.24164
Ho AM, Dion JM, Wong JC. Airway and Ventilatory Management Options in Congenital Tracheoesophageal Fistula Repair. J Cardiothorac Vasc Anesth. 2016;30(2):515-20. doi:10.1053/j.jvca.2015.04.005
Alabbad SI, Shaw K, Puligandla PS, Carranza R, Bernard C, Laberge JM. The pitfalls of endotracheal intubation beyond the fistula in babies with type C esophageal atresia. Semin Pediatr Surg. 2009;18(2):116-8. doi:10.1053/j.sempedsurg.2009.02.011
Ho AM, Wong JC, Chui PT, Karmakar MK. Case report: Use of two balloon-tipped catheters during thoracoscopic repair of a type C tracheoesophageal fistula in a neonate. Can J Anaesth. 2007;54(3):223-6. doi:10.1007/BF03022644
Ratan SK, Rattan KN, Ratan J, Bhatia V, Sodhi PK, Bhatia M. Temporary transgastric fistula occlusion as salvage procedure in neonates with esophageal atresia with wide distal fistula and moderate to severe pneumonia. Pediatr Surg Int. 2005;21(7):527-31. doi:10.1007/s00383-005-1407-8
Richenbacher WE, Ballantine TV. Esophageal atresia, distal tracheoesophageal fistula, and an air shunt that compromised mechanical ventilation. J Pediatr Surg. 1990;25(12):1216-8. doi:10.1016/0022-3468(90)90507-6
Pepper VK, Boomer LA, Thung AK, Grischkan JM, Diefenbach KA. Routine Bronchoscopy and Fogarty Catheter Occlusion of Tracheoesophageal Fistulas. J Laparoendosc Adv Surg Tech A. 2017;27(1):97-100. doi:10.1089/lap.2015.0607
Stollar F, Glangetas A, Luterbacher F, Gervaix A, Barazzone-Argiroffo C, Galetto-Lacour A. Frequency, Timing, Risk Factors, and Outcomes of Desaturation in Infants With Acute Bronchiolitis and Initially Normal Oxygen Saturation. JAMA Netw Open. 2020;3(12):e2030905. doi:10.1001/jamanetworkopen.2020.30905
Polito A, Patorno E, Costello JM, Salvin JW, Emani SM, Rajagopal S, et al. Perioperative factors associated with prolonged mechanical ventilation after complex congenital heart surgery. Pediatr Crit Care Med. 2011;12(3):e122-6. doi:10.1097/PCC.0b013e3181e912bd
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123(1):110-8. doi:10.1067/mtc.2002.119064
Jenkins KJ, Gauvreau K. Center-specific differences in mortality: Preliminary analyses using the Risk Adjustment in Congenital Heart Surgery (RACHS-1) method. J Thorac Cardiovasc Surg. 2002;124(1):97-104. doi:10.1067/mtc.2002.122311
Diaz LK, Akpek EA, Dinavahi R, Andropoulos DB. Tracheoesophageal fistula and associated congenital heart disease: implications for anesthetic management and survival. Paediatr Anaesth. 2005;15(10):862-9. doi:10.1111/j.1460-9592.2005.01582.x
Sanphasitvong V, Jim LY, Tantiwongkosri K. Impact of Accuracy of Preoperative Transthoracic Echocardiography on Complex Congenital Heart Surgery in Pediatrics. Siriraj Med J. 2019;71(6):480-5. https://doi.org/10.33192/Smj.2019.71
Andropoulos DB, Rowe RW, Betts JM. Anaesthetic and surgical airway management during tracheo-oesophageal fistula repair. Paediatr Anaesth. 1998;8(4):313-9. doi:10.1046/j.1460-9592.1998.00734.x
Atzori P, Iacobelli BD, Bottero S, Spirydakis J, Laviani R, Trucchi A, et al. Preoperative tracheobronchoscopy in newborns with esophageal atresia: does it matter? J Pediatr Surg. 2006;41(6):1054-57. doi:10.1016/j.jpedsurg.2006.01.074
Reeves ST, Burt N, Smith CD. Is it time to reevaluate the airway management of tracheoesophageal fistula? Anesth Analg. 1995;81(4):866-9. doi:10.1097/00000539-199510000-00036
Tabib A, Abrishami SE, Mahdavi M, Mortezaeian H, Totonchi Z. Predictors of Prolonged Mechanical Ventilation in Pediatric Patients After Cardiac Surgery for Congenital Heart Disease. Res Cardiovasc Med. 2016;5(3):e30391. doi:10.5812/cardiovascmed.30391
Friedmacher F, Kroneis B, Huber-Zeyringer A, Schober P, Till H, Sauer H, et al. Postoperative Complications and Functional Outcome after Esophageal Atresia Repair: Results from Longitudinal Single-Center Follow-Up. J Gastrointest Surg. 2017;21(6):927-35. doi:10.1007/s11605-017-3423-0
Lal DR, Gadepalli SK, Downard CD, Ostlie DJ, Minneci PC, Swedler RM, et al. Challenging surgical dogma in the management of proximal esophageal atresia with distal tracheoesophageal fistula: Outcomes from the Midwest Pediatric Surgery Consortium. J Pediatr Surg. 2018;53(7):1267-72. doi:10.1016/j.jpedsurg.2017.05.024
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














