Perceptions and Management Practices of Onychomycosis Among Thai Physicians
DOI:
https://doi.org/10.33192/smj.v75i2.260741Keywords:
Mycological laboratory, general practitionersAbstract
Objective: To examine the proportion of physicians who conducted mycological laboratory procedures to confirm a diagnosis of onychomycosis. The secondary purpose was to evaluate the practical management of physicians, comparing general practitioners and dermatology-related physicians.
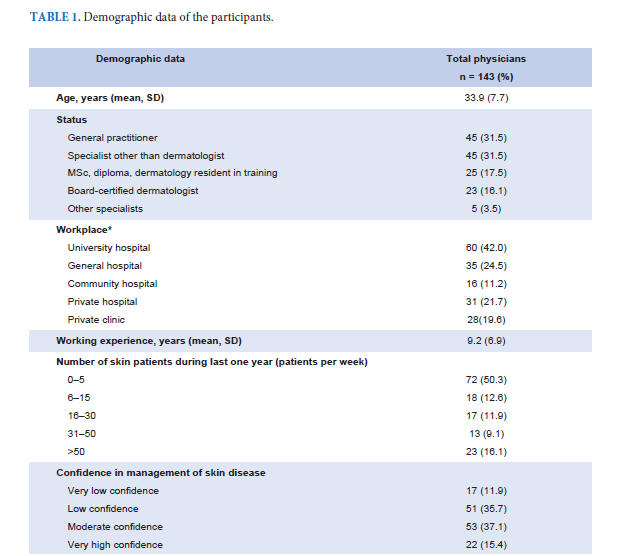
Materials and Methods: This cross-sectional study and questionnaire-based research was conducted during 2021-2022. The questionnaire was composed of questions related to the practical management of onychomycosis, including diagnosis and treatment.
Results: Overall, 143 physicians were recruited to take part in this study. The number of physicians who conducted direct examination with potassium hydroxide was 99 (69.2%). The number of dermatology-related physicians who conducted mycological laboratory examinations to confirm the diagnosis was significantly higher than among general physicians (95.8% vs. 52.2%; p<0.001). Feet examination and determination of poor prognostic factors, such as elderly age, nail thickness, presence of dermatophytoma and nondermatophytes infection, were done by the dermatology-related physicians in significantly higher numbers. Blood testing before starting treatment for onychomycosis with oral antifungal medications seemed to be higher (87.5%) in the dermatology-related group. Moreover, mycological re-evaluation after treatment cessation was more significantly requested by the dermatologyrelated participants (75% vs. 15.8%, p<0.001).
Conclusion: Laboratory confirmation, feet examination, and the recognition of poor prognostic factors were significantly lower in the general practitioner group. These findings should raise awareness for improving further education about onychomycosis management in medical students, since mycological laboratory examination is crucial for diagnosis and it is helpful in guiding the proper disease management for complete disease remission.
References
Sigurgeirsson B, Baran R. The prevalence of onychomycosis in the global population: a literature study. J Eur Acad Dermatol Venereol. 2014;28(11):1480-91.
Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists’ guidelines for the management of onychomycosis 2014. Br J Dermatol. 2014;171(5):937-58.
Denning DW, Evans EG, Kibbler CC, Richardson MD, Roberts MM, Rogers TR, et al. Fungal nail disease: a guide to good practice (report of a Working Group of the British Society for Medical Mycology). BMJ. 1995;311(7015):1277-81.
Bunyaratavej S, Prasertworonun N, Chaiwanon O, Pattanaprichakul P. Alarming trend towards deviation of clinical diagnosis and management of psoriatic nails by Thai general practitioners and non-dermatologist specialists. J Eur Acad Dermatol Venereol. 2015;29(2):398-9.
Wilcock M, Hartley J, Gould D. Inappropriate use of oral terbinafine in family practice. Pharm World Sci. 2003;25(1):25-6.
Gupta AK, Mays RR, Versteeg SG, Piraccini BM, Takwale A, Shemer A, et al. Global perspectives for the management of onychomycosis. Int J Dermatol. 2019;58(10):1118-29.
Lasseter G, McNulty CA, Palmer M, Yoxall H, Kibbler C, Health Protection Agency GPMLUG. Developing best practice for fungal specimen submission--fungal audit of general practice. Mycoses. 2012;55(6):476-82.
Wharry S. FDA issues warnings about drugs used to treat fungal nail infections. CMAJ. 2001;164(12):1738.
Gupta AK, Shear NH. A questionnaire study on the management of onychomycosis: a Canadian perspective. Int J Dermatol. 1998;37(6):457-60.
Walling HW. Subclinical onychomycosis is associated with tinea pedis. Br J Dermatol. 2009;161(4):746-9.
Loo DS. Onychomycosis in the elderly: drug treatment options. Drugs Aging. 2007;24(4):293-302.
Widaty S, Miranda E, Bramono K, Menaldi SL, Marissa M, Oktarina C, et al. Prognostic factors influencing the treatment outcome of onychomycosis Candida. Mycoses. 2020;63(1):71-7.
Xiang L, Lipner SR. Characteristics of malpractice lawsuits involving nail disorders in the United States from 1977 to 2019. J Am Acad Dermatol. 2020;83(4):1202-4.
Leeyaphan C, Bunyaratavej S, Chadchavalpanichaya N, Rujitharanawong C, Phaitoonwattanakij S, Matthapan L. Clinical and Laboratory Findings in Trauma-Induced Nail Dystrophy versus Onychomycosis. Siriraj Med J. 2018;70(6):490-5.
Published
How to Cite
Issue
Section
Categories
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














