Sleep Quality and Associated Factors in Elderly Patients with Type-2 Diabetes Mellitus
DOI:
https://doi.org/10.33192/smj.v75i5.260818Keywords:
sleep quality, poor sleep quality, diabetes mellitus type 2, geriatric, older adultAbstract
Objective: The prevalence of poor sleep quality has been greatly escalating over the past years, along with the surging of type 2 Diabetes Mellitus (DM). The aging population is most concerned as sleep quality is notably impaired and influences the diabetic condition. This study aimed to observe the sleep quality and factors related to poor sleep quality in elderly patients with type-2 DM.
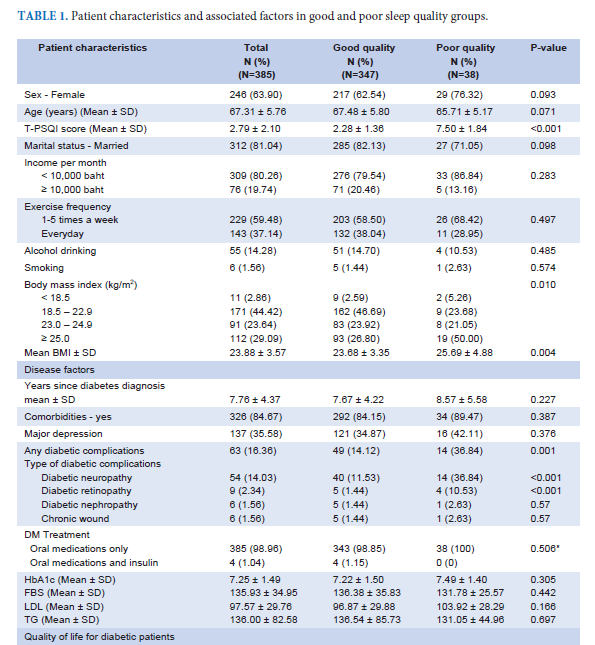
Materials and Methods: A cross-sectional study of patients with type 2 DM, aged 60 years and above was conducted. The questionnaires included demographic data, the Thai version of the Pittsburgh Sleep Quality Index (T-PSQI), the Thai version of the Diabetic-39, and the Thai Geriatric Depression Scale-15. Factors associated with sleep quality were analyzed using the logistic regression model.
Results: Among 385 participants with a mean age of 67 years old was 63.90% female. The prevalence of poor sleep quality was 9.88%. No association was found between sleep quality and glycemic levels. The related factors for poor sleep quality were sex (aOR = 2.57, p = 0.035, 95%CI = 1.06-5.93), body mass index (aOR =1.09, p = 0.028, 95% CI = 1.00-1.20), and diabetic complications. Diabetic retinopathy showed highest odd ratio (aOR = 6.28, p = 0.021, 95% CI = 1.32-29.94).
Conclusion: The prevalence of poor sleep quality was low in the current study. We found a strong association between diabetic complications and poor sleep quality. Evaluation of sleep quality may help to enhance overall health and care for diabetic geriatric patients.
References
Khorasani ZM, Ravan VR, Hejazi S. Evaluation of the Prevalence of Sleep Disorder Among Patients with Type 2 Diabetes Mellitus Referring to Ghaem Hospital from 2016 to 2017. Curr Diabetes Rev. 2021;17(2):214-21.
Ogunbode AM, Adebusoye LA, Olowookere OO, Owolabi M, Ogunniyi A. Factors Associated with Insomnia among Elderly Patients Attending a Geriatric Centre in Nigeria. Curr Gerontol Geriatr Res. 2014;2014:780535.
Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213.
3rd CFR, O'Hara R. DSM-5 Sleep-Wake Disorders Classification: Overview for Use in Clinical Practice. Am J Psychiatry. 2013;170(10):1099-101.
Yoshida K, Otaka H, Murakami H, Nakayama H, Murabayashi M, Mizushiri S, et al. Association between insomnia and coping style in Japanese patients with type 2 diabetes mellitus. Neuropsychiatr Dis Treat. 2018;14:1803-9.
Tufan A, Ilhan B, Bahat G, Karan MA. An under-diagnosed geriatric syndrome: sleep disorders among older adults. Afr Health Sci. 2017;17(2):436-44.
Zhu B-Q, Li X-M, Wang D, Yu X-F. Sleep quality and its impact on glycaemic control in patients with type 2 diabetes mellitus. International Journal of Nursing Sciences. 2014;1(3):260-5.
Birhanu TE, Getachew B, Gerbi A, Dereje D. Prevalence of poor sleep quality and its associated factors among hypertensive patients on follow up at Jimma University Medical Center. J Hum Hypertens. 2021;35(10):94-100.
McClellan SP, Haque K, Garcia-Pena C. Diabetes multimorbidity combinations and disability in the Mexican Health and Aging Study, 2012-2015. Arch Gerontol Geriatr. 2021;93:104292.
Leproult R, Deliens G, Gilson M, Peigneux P. Beneficial impact of sleep extension on fasting insulin sensitivity in adults with habitual sleep restriction. Sleep. 2015;38(5):707-15.
Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol (1985). 2005;99(5):2008-19.
Krishnasamy S, Abell TL. Diabetic Gastroparesis: Principles and Current Trends in Management. Diabetes Ther. 2018;9(Suppl 1):1-42.
Luyster FS, Dunbar-Jacob J. Sleep quality and quality of life in adults with type 2 diabetes. Diabetes Educ. 2011;37(3):347-55.
Zuo X, Dong Z, Zhang P, Zhang P, Chang G, Xiang Q, et al. Effects of cognitive behavioral therapy on sleep disturbances and quality of life among adults with type 2 diabetes mellitus: A randomized controlled trial. Nutr Metab Cardiovasc Dis. 2020;30(11):1980-8.
Edmealem A, Degu SG, Haile D, Gedfew M, Bewket B, Andualem A. Sleep Quality and Associated Factors among Diabetes, Hypertension, and Heart Failure Patients at Debre Markos Referral Hospital, Northwest Ethiopia. Sleep Disord. 2020;2020:6125845.
Sitasuwan T, Bussaratid S, Ruttanaumpawan P, Chotinaiwattarakul W. Reliability and validity of the Thai version of the Pittsburgh Sleep Quality Index. J Med Assoc Thai. 2014;97 Suppl 3:S57-67.
Songraksa K, Lerkiatbundit S. Development of a disease specific quality of life instrument: Thai version of the Diabetic-39. Songkla Med J. 2009;27(1):35-49.
Wongpakaran N, Wongpakaran T, Reekum RV. The Use of GDS-15 in detecting MDD: a comparison between residents in a Thai long-term care home and geriatric outpatients. J Clin Med Res. 2013;5(2):101-11.
Sheehan P, Jones P, Giurini JM, Caselli A, Veves A. Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Plast Reconstr Surg. 2006;117(7 Suppl):239S-44S.
Sridhar GR, Madhu K. Prevalence of sleep disturbances in diabetes mellitus. Diabetes Res Clin Pract. 1994;23(3):183-6.
Gu D, Sautter J, Pipkin R, Zeng Y. Sociodemographic and health correlates of sleep quality and duration among very old Chinese. Sleep. 2010;33(5):601-10.
Telford O, Diamantidis CJ, Bosworth HB, Patel UD, Davenport CA, Oakes MM, et al. The relationship between Pittsburgh Sleep Quality Index subscales and diabetes control. Chronic Illness. 2018;15(3):210-9.
Grandner MA, Sands-Lincoln MR, Pak VM, Garland SN. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013;5:93-107.
Tang J, Kern TS. Inflammation in diabetic retinopathy. Prog Retin Eye Res. 2011;30(5):343-58.
Tan NYQ, Chew M, Tham Y-C, Nguyen QD, Yasuda M, Cheng C-Y, et al. Associations between sleep duration, sleep quality and diabetic retinopathy. PLoS One. 2018;13(5):e0196399.
Situm M, Kolić M, Spoljar S. Quality of Life and psychological aspects in Patients with Chronic leg ulcer. Acta Med Croatica. 2016;70(1):61-3.
Rungmanee S, Banhiran W, Keskool P, Assanasen P, Chotinaiwattarakul W, Nujchanart N. Characteristics and Clinical Presentations of Patients at the Siriraj Snoring Clinic. Siriraj Med J. 2020;72(3):202-8.
Wongwutthiwet P, Bosittipichet T, Leesri T. The Efficacy of Follow-up Phone Calls for Capillary Blood Glucose Lowering in Diabetic Patients in Primary Care Unit. Siriraj Med J. 2021;73(12):801-7.
Downloads
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














