A Survey of Daily Genital Care Practices among Reproductive-aged Female Personnel at Siriraj Hospital
DOI:
https://doi.org/10.33192/smj.v75i4.260837Keywords:
survey, genital care, women, reproductive aged women, ThaiAbstract
Objective: To demonstrate the genital cleansing habit and associating factors among reproductive-aged Thai women.
Materials and Methods: The survey was conducted at Siriraj Hospital between June and September 2022 (COA no. Si 370/2022). Twenty patient unit wards and 20 office units were randomly selected. Only active Siriraj female staff aged 18-50 were approached. The exclusion criteria included medical students and doctors, pregnant women, incomplete questionnaires, and women with immunocompromised conditions. Twenty sets of questionnaires, together with an information sheet as well as a box to return the questionnaire, were left at each unit. The primary outcome was the frequency of daily genital cleansing done outside of shower time. Associating factors and other genital care practices were secondary outcomes.
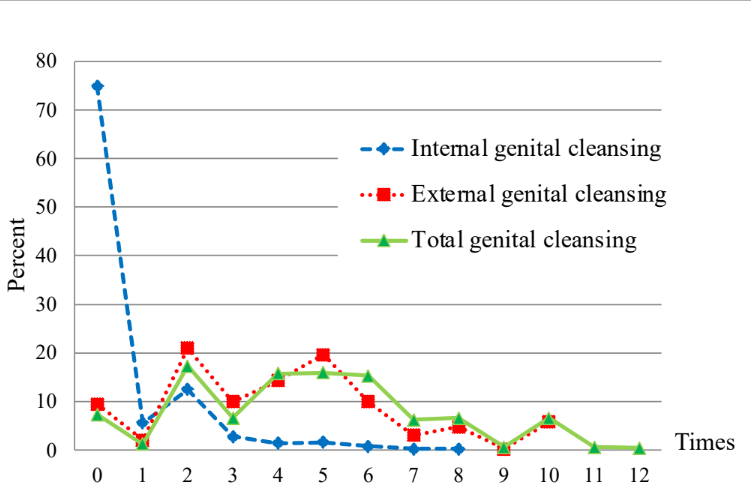
Results: Of the 800 distributed questionnaires, 611 were returned (response rate of 76.4%) and 504 were eligible for the study. The participants were 32.7±7.3 years old and most were in the 25-40 age group. Up to 90% reported genital cleansing outside shower time and 74.2% (374/504) of all respondents and 74.7% (236/316) of those with sexual experience cleansed >2 times daily. Twenty-four participants (4.8%) practiced vaginal douche. Water without genital care products is the most common method of cleansing. There was no association between sexual health risks and frequency of cleansing.
Conclusion: Three fourths of reproductive aged Thai women practice genital cleansing >2 times per day. Water without genital care products is the most common method of cleansing. There is no association between the habit and any demographic data and sexual health risks.
References
Amabebe E, Anumba DOC. The Vaginal Microenvironment: The Physiologic Role of Lactobacilli. Front Med (Lausanne) 2018;5:181.
Chen Y, Bruning E, Rubino J, Eder SE. Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage. Women's Health 2017;13:58-67.
Yudin M, Money D. Screening and management of bacterial vaginosis in pregnancy. J Obstet Gynaecol Can 2008;30:702-8.
Freitas A, Bocking A, Hill J, Money D. Increased richness and diversity of the vaginal microbiota and spontaneous preterm birth. Microbiome 2018;6:117.
Paramel Jayaprakash T, Wagner E, van Schalkwyk J, Albert A, Hill J, Money D. High diversity and variability in the vaginal microbiome in women following preterm premature rupture of membranes (PPROM): A prospective cohort study. PLoS One 2016;11:11.
Canadian Women's Health Network. Keeping your vagina healthy 2006. Available from: http://www.cwhn.ca/node/40797. (Accessed 14 December 2022)
Chayachinda C, Thamkhantho M, Chalermchockcharoenkit M, Nuengton C, Thipmontree W. Characteristics of Clients at the Siriraj Female STD Clinic during 2011-2015. Siriraj Medical Bulletin 2018;11:182-9.
Chayachinda C, Chinhiran K, Kittiyaowamarn R, Chaithongwongwatthana S, Teeratakulpisarn N. The Thai 2022 Sexually Transmitted Infections Treatment Guideline: Abnormal vaginal discharge Thai J Obstet Gynaecol 2022;30:222-33
Atashili J, Poole C, Ndumbe PM, Adimora AA, Smith JS. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS 2008;22:1493-501.
Cherpes TL, Meyn LA, Krohn MA, Lurie JG, Hillier SL. Association between acquisition of herpes simplex virus type 2 in women and bacterial vaginosis. Clin Infect Dis 2003;37:319-25.
Haggerty CL, Hillier SL, Bass DC, Ness RB, Evaluation PID, Clinical Health study i. Bacterial vaginosis and anaerobic bacteria are associated with endometritis. Clin Infect Dis 2004;39:990-5.
Hillier SL, Krohn MA, Cassen E, Easterling TR, Rabe LK, Eschenbach DA. The role of bacterial vaginosis and vaginal bacteria in amniotic fluid infection in women in preterm labor with intact fetal membranes. Clin Infect Dis 1995;20 Suppl 2:S276-8.
Donders GG, Van Calsteren K, Bellen G, Reybrouck R, Van den Bosch T, Riphagen I, et al. Predictive value for preterm birth of abnormal vaginal flora, bacterial vaginosis and aerobic vaginitis during the first trimester of pregnancy. BJOG 2009;116:1315-24.
Ruiz C, Giraldo P, Sanches J, Reis V, Beghini J, Laguna C, et al. Daily genital cares of female gynecologists: a descriptive study. Rev Assoc Med Bras 2019;65:171-6.
Crann S, Cunningham S, Albert A, Money D, O'Doherty K. Vaginal health and hygiene practices and product use in Canada: a national cross-sectional survey. BMC Womens Health 2018;18:52.
Aslan E, Bechelaghem N. To 'douche' or not to 'douche': hygiene habits may have detrimental effects on vaginal microbiota. J Obstet Gynaecol 2018;38:678-81.
Chandra A, Martinez G, Mosher W, Abma J, Jones J. Fertility,family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Statistics 2005;23:1-160.
Cottrell B, Close F. Vaginal douching among university womenin the southeastern United States. Journal of American College Health 2008;56:415-21.
Suwanrattanadech S, Lertbunnaphong T, Boriboonhirunsarn D. Use of feminine hygiene products in Thai women. Siriraj Med J 2011;63:111–4.
Grimley D, Annang L, Foushee H, Bruce F, Kendrick J. Vaginal douches and other feminine hygiene products: women's practices and perceptions of product safety. Matern Child Health J 2006;10:303-10.
Chayachinda C, Rekhawasin T. Reproductive outcomes of patients being hospitalised with pelvic inflammatory disease. J Obstet Gynaecol 2017;37:228-32.
Panchalee T, Chayachinda C, Panyakat W, Chen M, Quinones-Garcia V, Pernsoongnern P. Characteristics and neonatal outcomes of teenage pregnant Women diagnosed with syphilis at Siriraj Hospital. Siriraj Med J 2018;70:298-301.
Chayachinda C. A decade of fighting vulvovaginal candidiasis and bacterial vaginosis: The latest real-world study in Thailand with the clotrimazole and lactic acid. RTCOG 2022 meeting: Now and Beyond; Pattaya, Chonburi, Thailand2022.
Javed A, Parvaiz F, Manzoor S. Bacterial vaginosis: an insight into the prevalence, alternative treatments regimen and it's associated resistance patterns. Microb Pathog 2019;127:21-30.
Ott M, Ofner S, Fortenberry J. Beyond Douching: Use of Feminine Hygiene Products and STI Risk among Young Women. J Med Sex 2009;6:1335-40.
Arab H, Almadani L, Tahlak M. The Middle East and Central Asia guidelines on female genital hygiene. BMJ Middle East 2011;19: 99-106.
Royal College of General Practitioners. The management of vulval skin disorders, http://www.snhcic.org.uk/assets/cms_page_media/211/RCOG%20-%20Vulval%20Skin%20 Disorders.pdf (Accessed 9 January 2023).
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














