Factors Associated with Cervical Cancer Screening Overuse and Underuse, and Attitude towards Human Papillomavirus Self-sampling among Hospital Staffs
DOI:
https://doi.org/10.33192/smj.v75i3.260868Keywords:
Attitude, human papillomavirus cervical self-sampling, cervical cancer screening overuse and underuse, female staff membersAbstract
Objective: To investigate the rates of and factors associated with cervical cancer screening overuse and underuse, and the attitude towards human papillomavirus (HPV) self-sampling among hospital staffs.
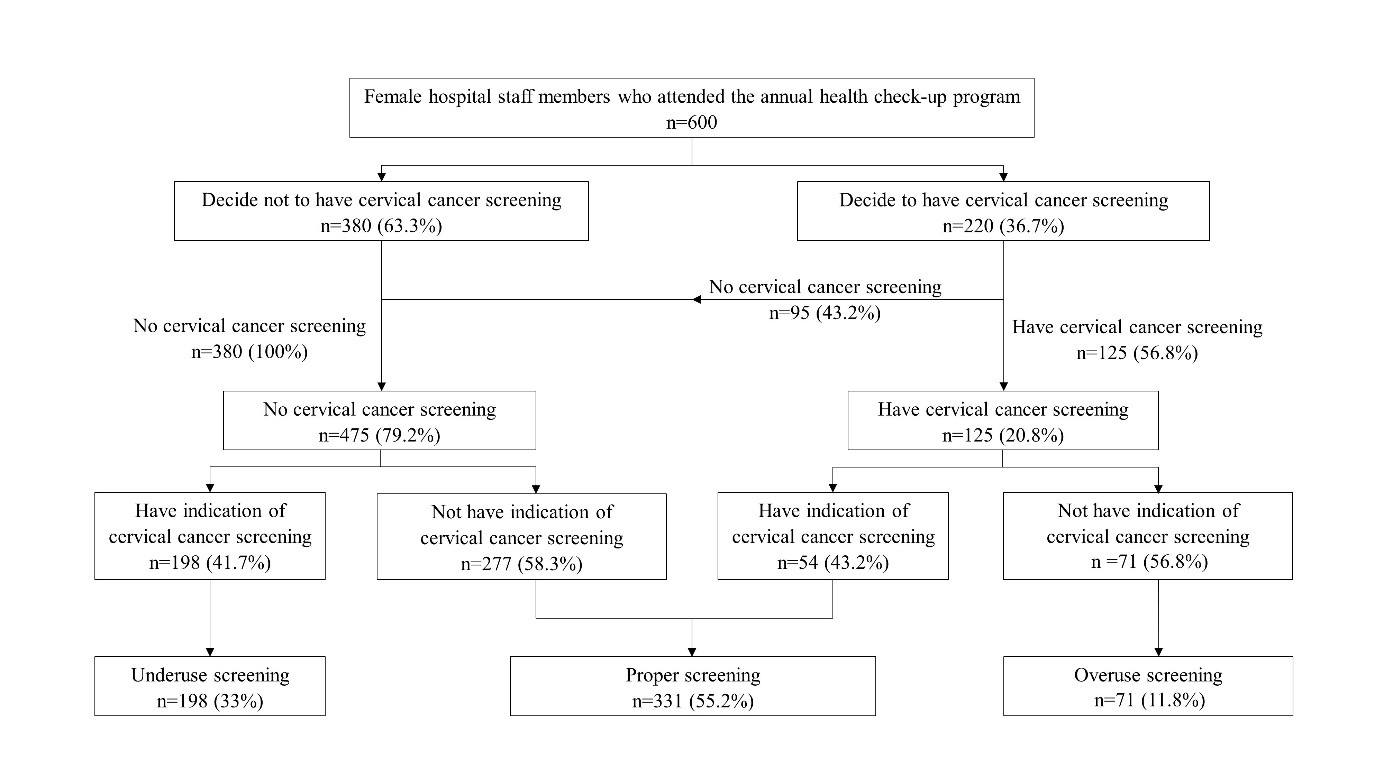
Materials and Methods: This cross-sectional study included female hospital staff undergoing an annual health check-up. A questionnaire was used to collect sociodemographic characteristics, indication for cervical cancer screening, reasons for screening decision, and attitude toward HPV self-sampling. Screening overuse was defined as having cervical cancer screening without indication while screening underuse was having indication for screening but not receiving it.
Results: Among the 600 included participants, 220 and 380 women decided to screen and not to screen for cervical cancer, respectively. The prevalence of screening overuse and underuse was 11.8% and 33.0%, respectively. Multivariate analysis revealed age was associated with screening underuse (aOR: 1.06, 95% CI: 1.04-1.09; p<0.001), whereas married status was associated with screening overuse (aOR: 3.73, 95% CI: 2.05-6.79; p<0.001). The common reasons for screening were “add-on to annual health check-up” (93.2%), “fear of cancer” (84.1%), and “family/organizational support” (54.5%). The common reasons for not screening were “feeling healthy” (73.7%), “fear of pain” (58.7%), and “embarrassment” (57.1%). Most women (65.1%) expressed interest in screening via HPV self-sampling.
Conclusion: Overuse and underuse of cervical cancer screening were common. An accurate information regarding screening indication should be provided and indication restriction should be implemented to a health system to avoid screening overuse. In addition, an encouragement should be enhanced to the target population to attend the screening program.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-49.
Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Pineros M, Znaor A, et al. Cancer statistics for the year 2020: An overview. Int J Cancer. 2021;149(4):778-89.
Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49(15):3262-73.
Mukem S, Meng Q, Sriplung H, Tangcharoensathien V. Low Coverage and Disparities of Breast and Cervical Cancer Screening in Thai Women: Analysis of National Representative Household Surveys. Asian Pac J Cancer Prev. 2015;16(18):8541-51.
Niu L, Virani S, Bilheem S, Sriplung H. The effect of Pap smear screening on cervical cancer stage among southern Thai women. Sci Rep. 2019;9(1):16921.
Ifemelumma CC, Anikwe CC, Okorochukwu BC, Onu FA, Obuna JA, Ejikeme BN, et al. Cervical Cancer Screening: Assessment of Perception and Utilization of Services among Health Workers in Low Resource Setting. Int J Reprod Med. 2019;2019:6505482.
Chittithaworn S, Charakorn C, Kongsawatvorakul C. Cervical Cancer Screening Guidelines: An updated review. Thai Journal of Obstetrics and Gynaecology. 2021;29:186-90.
Parekh N, Donohue JM, Men A, Corbelli J, Jarlenski M. Cervical Cancer Screening Guideline Adherence Before and After Guideline Changes in Pennsylvania Medicaid. Obstet Gynecol. 2017;129(1):66-75.
Almeida CM, Rodriguez MA, Skootsky S, Pregler J, Steers N, Wenger NS. Cervical cancer screening overuse and underuse: patient and physician factors. Am J Manag Care. 2013;19(6):482-9.
Wright JD, Chen L, Tergas AI, Melamed A, St Clair CM, Hou JY, et al. Overuse of Cervical Cancer Screening Tests Among Women With Average Risk in the United States From 2013 to 2014. JAMA Netw Open. 2021;4(4):e218373.
Dillner J, Rebolj M, Birembaut P, Petry KU, Szarewski A, Munk C, et al. Long term predictive values of cytology and human papillomavirus testing in cervical cancer screening: joint European cohort study. BMJ. 2008;337:a1754.
Sasieni P, Adams J, Cuzick J. Benefit of cervical screening at different ages: evidence from the UK audit of screening histories. Br J Cancer. 2003;89(1):88-93.
Kulasingam SL, Havrilesky L, Ghebre R, Myers ER. Screening for Cervical Cancer: A Decision Analysis for the US Preventive Services Task Force. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Rockville (MD)2011.
Stout NK, Goldhaber-Fiebert JD, Ortendahl JD, Goldie SJ. Trade-offs in cervical cancer prevention: balancing benefits and risks. Arch Intern Med. 2008;168(17):1881-9.
Practice Bulletin No. 168: Cervical Cancer Screening and Prevention. Obstet Gynecol. 2016;128(4):e111-e30.
Fontham ETH, Wolf AMD, Church TR, Etzioni R, Flowers CR, Herzig A, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70(5):321-46.
Ronco G, Dillner J, Elfstrom KM, Tunesi S, Snijders PJ, Arbyn M, et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet. 2014;383(9916):524-32.
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla Palma P, Del Mistro A, et al. Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol. 2010;11(3):249-57.
Moscicki AB, Shiboski S, Hills NK, Powell KJ, Jay N, Hanson EN, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet. 2004;364(9446):1678-83.
Darwish-Yassine M, Garvin AD, Johnston CM, Zoschnick L, Conners A, Laing S, et al. An assessment of gynecological cytology screening practices among health care providers nationwide. Arch Pathol Lab Med. 2015;139(5):650-5.
Gerend MA, Shepherd MA, Kaltz EA, Davis WJ, Shepherd JE. Understanding women's hesitancy to undergo less frequent cervical cancer screening. Prev Med. 2017;95:96-102.
Rendle KA, Schiffman M, Cheung LC, Kinney WK, Fetterman B, Poitras NE, et al. Adherence patterns to extended cervical screening intervals in women undergoing human papillomavirus (HPV) and cytology cotesting. Prev Med. 2018;109:44-50.
Singh E, Seth S, Rani V, Srivastava DK. Awareness of cervical cancer screening among nursing staff in a tertiary institution of rural India. J Gynecol Oncol. 2012;23(3):141-6.
Srisubat A, Limwattanayingyong A, Chaisewikul R, Anannamcharoen S. Factors Affecting the Utilization of Pap Smear Screening Program among Nurses in the Department of Medicine, Siriraj Hospital. Siriraj Medical Journal. 2006;58(8):1002-5.
Yeh PT, Kennedy CE, de Vuyst H, Narasimhan M. Self-sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis. BMJ Glob Health. 2019;4(3):e001351.
Tota JE, Bentley J, Blake J, Coutlee F, Duggan MA, Ferenczy A, et al. Introduction of molecular HPV testing as the primary technology in cervical cancer screening: Acting on evidence to change the current paradigm. Prev Med. 2017;98:5-14.
Madzima TR, Vahabi M, Lofters A. Emerging role of HPV self-sampling in cervical cancer screening for hard-to-reach women: Focused literature review. Can Fam Physician. 2017;63(8):597-601.
Bais AG, van Kemenade FJ, Berkhof J, Verheijen RH, Snijders PJ, Voorhorst F, et al. Human papillomavirus testing on self-sampled cervicovaginal brushes: an effective alternative to protect nonresponders in cervical screening programs. Int J Cancer. 2007;120(7):1505-10.
Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360(14):1385-94.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














