Assessment of Volume Status in Chronic Hemodialysis: Comparison of Lung Ultrasound to Clinical Practice and Bioimpedance
DOI:
https://doi.org/10.33192/smj.v75i3.261016Keywords:
lung ultrasonography, extravascular lung water, hemodialysis, all-cause mortality, morbidities, intradialytic complicationsAbstract
Objective: To compare LUS with other volume assessment methods, and to verify the prognostic value of LUS in Thai chronic HD patients.
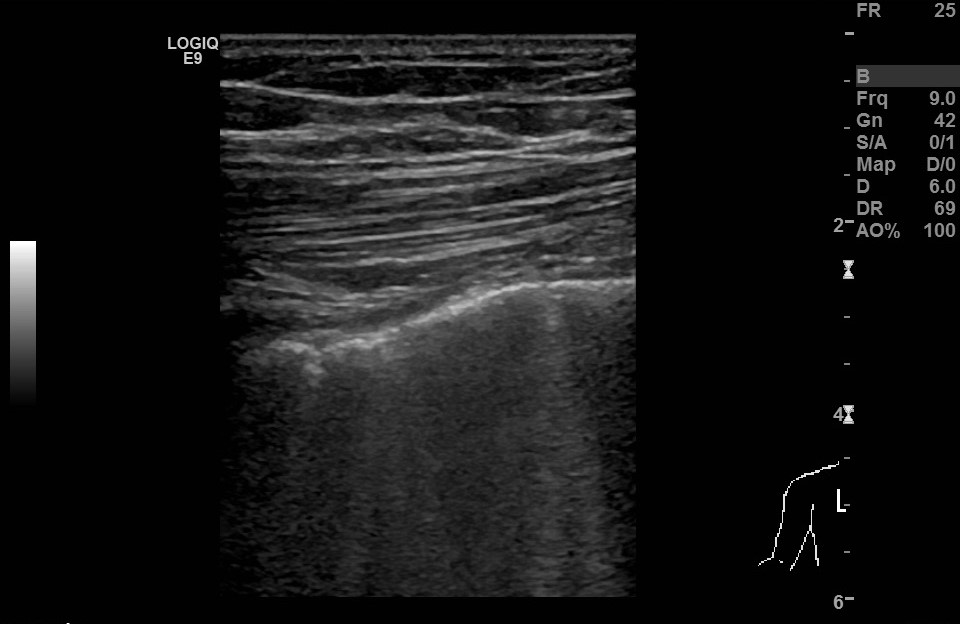
Materials and Methods: We conducted a prospective cohort study in 36 chronic HD patients. Volume status before the HD session was evaluated by physical examinations, bioimpedance analysis (BIA), and ultrasound lung comets (ULCs). Mortality and morbidities were recorded during a 1-year follow-up period.
Results: The degree of lung fluid accumulation was assessed by summation of the number of ULCs, and was classified into 3 groups: mild-to-moderate (ULC<15–29), severe (ULC=30–59), and very severe (ULC>60) in 11.1%, 77.8%, and 11.1% of the patients, respectively. Either clinical edema or lung crackle had low sensitivity (20-32%) to detect extravascular lung water excess in patient with mild-to-moderate ULC and severe ULC. Overhydration assessed by BIA was found in 75% and 64.3% of patients with mild-to-moderate and severe ULC, respecively. In patients with very severe ULC, the admission rate due to volume overload was significantly higher, there was also a trend of increased mortality, as well as intradialytic complications.
Conclusion: Clinical assessment and BIA have limited value in determining extravascular fluid excess in the lung. Lung ultrasound is a useful tool to detect subclinical pulmonary congestion. The long-term outcome by using LUS-guided fluid management needs larger population studies.
References
Lumpaopong A, Chuasuwan A. Thailand Renal Replacement Therapy Year 2016-2019. The Nephrology Society of Thailand. 2019:1-64.
Kalantar-Zadeh K, Regidor DL, Kovesdy CP, Van Wyck D, Bunnapradist S, Horwich TB, et al. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009;119(5):671-9.
Lee MJ, Doh FM, Kim CH, Koo HM, Oh HJ, Park JT, et al. Interdialytic weight gain and cardiovascular outcome in incident hemodialysis patients. Am J Nephrol. 2014;39(5):427-35.
Torino C, Gargani L, Sicari R, Letachowicz K, Ekart R, Fliser D, et al. The Agreement between Auscultation and Lung Ultrasound in Hemodialysis Patients: The LUST Study. Clinical journal of the American Society of Nephrology : Clin J Am Soc Nephrol. 2016;11(11):2005-11.
Kotanko P, Levin NW, Zhu F. Current state of bioimpedance technologies in dialysis. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2008;23(3):808-12.
Yilmaz Z, Yildirim Y, Aydin FY, Aydin E, Kadiroglu AK, Yilmaz ME, et al. Evaluation of fluid status related parameters in hemodialysis and peritoneal dialysis patients: Clinical usefulness of bioimpedance analysis. Medicina. 2014;50(5):269-74.
Lichtenstein DA. Lung ultrasound in the critically ill. Annals of intensive care. 2014;4(1):1.
Enghard P, Rademacher S, Nee J, Hasper D, Engert U, Jorres A, et al. Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients. Critical care. 2015;19:36.
Vitturi N, Dugo M, Soattin M, Simoni F, Maresca L, Zagatti R, et al. Lung ultrasound during hemodialysis: the role in the assessment of volume status. International urology and nephrology. 2014;46(1):169-74.
Zoccali C, Tripepi R, Torino C, Bellantoni M, Tripepi G, Mallamaci F. Lung congestion as a risk factor in end-stage renal disease. Blood purification. 2013;36(3-4):184-91.
Zoccali C, Torino C, Tripepi R, Tripepi G, D'Arrigo G, Postorino M, et al. Pulmonary congestion predicts cardiac events and mortality in ESRD. J Am Soc Nephrol 2013;24(4):639-46.
Siriopol D, Hogas S, Voroneanu L, Onofriescu M, Apetrii M, Oleniuc M, et al. Predicting mortality in haemodialysis patients: a comparison between lung ultrasonography, bioimpedance data and echocardiography parameters. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2013;28(11):2851-9.
Kataoka H, Matsuno O. Age-related pulmonary crackles (rales) in asymptomatic cardiovascular patients. Annals of family medicine. 2008;6(3):239-45.
Frassi F, Gargani L, Tesorio P, Raciti M, Mottola G, Picano E. Prognostic value of extravascular lung water assessed with ultrasound lung comets by chest sonography in patients with dyspnea and/or chest pain. Journal of cardiac failure. 2007;13(10):830-5.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440-63.
Flythe JE, Chang TI, Gallagher MP, Lindley E, Madero M, Sarafidis PA, et al. Blood pressure and volume management in dialysis: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2020;97(5):861-76.
Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944-56.
Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JE, Cleland JG, et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail. 2010;12(5):423-33.
Platz E, Lewis EF, Uno H, Peck J, Pivetta E, Merz AA, et al. Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J 2016;37(15):1244-51.
Ngoh CLY, Teng HL, Chua YT, Leo CCH, Wong WK. Comparison between lung ultrasonography and current methods for volume assessment in Asian chronic hemodialysis patients. Hemodial Int. 2020;24(4):516-27.
Banerjee D, Ma JZ, Collins AJ, Herzog CA. Long-term survival of incident hemodialysis patients who are hospitalized for congestive heart failure, pulmonary edema, or fluid overload. Clin J Am Soc Nephrol 2007;2(6):1186-90.
Mallamaci F, Benedetto FA, Tripepi R, Rastelli S, Castellino P, Tripepi G, et al. Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging. 2010;3(6):586-94.
Loutradis C, Sarafidis PA, Ferro CJ, Zoccali C. Volume overload in hemodialysis: diagnosis, cardiovascular consequences, and management. Nephrol Dialy Transplant 20121; 36(12):2182-93.
Saad MM, Kamal J, Moussaly E, Karam B, Mansour W, Gobran E, et al. Relevance of B-lines on lung ultrasound in volume overload and pulmonary congestion: Clinical correlations and outcomes in patients on hemodialysis. Cardiorenal Med 2018; 8(2): 83-91.
Downloads
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














