Specific Learning Objectives in the Form of Selfassessment to Facilitate Rehabilitation Residency Training Competency: A Prospective Cohort Study
DOI:
https://doi.org/10.33192/smj.v75i4.261160Keywords:
Learning objectives, Residency training, Self-assessmentAbstract
Objectives: To explore the benefits of rotation- and milestone-specific learning objectives in the form of self-assessment questionnaires to facilitate rehabilitation residency training.
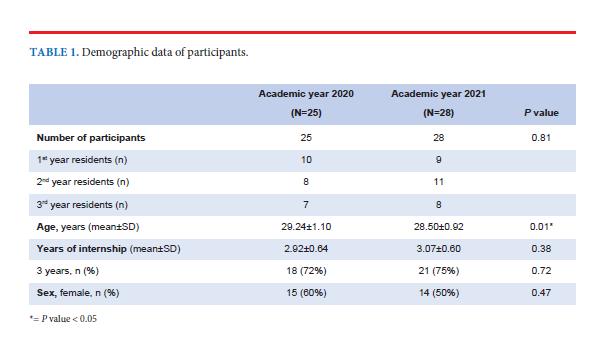
Materials and methods: Control and intervention groups were formed during academic years 2020 and 2021, respectively. The group participants were residents undergoing training in rehabilitation medicine. Before entering their rotations, the intervention group participants were provided rotation- and milestone-specific learning objectives in the form of self-assessment questionnaires. The participants of both groups self-assessed their confidence levels for each learning objective after the rotations, using a 5-level Likert scale. The self-rated scores of the 2 groups were compared.
Results: Twenty-five and 28 residents were enrolled in control and intervention groups, respectively. There were 12 sets of learning objectives (4 rotations; 3 milestones). Only 2 sets revealed higher self-rated scores for the intervention group (the pediatric and the pain rotations of the second-year residents). The groups’ scores for Entrustable Professional Activities (EPAs) and tests of participants’ knowledge of the learning objectives showed no differences.
Conclusions: Providing learning objectives and conducting self-assessments are crucial for successful learning. Although there is limited evidence of the benefits of our intervention, the advantages of specific learning objectives might be enhanced when combined with other measures that support residency training.
References
The Board of Training and Examination in Rehabilitation Medicine The Royal College of Physiatrists of Thailand. Residency Training Curriculum in Rehabilitation Medicine [Internet]. Chiangmai (TH); 2019 [updated 2019; cited 2023 Feb 2] Available from: http://rehabmed.or.th/main/wp-content/uploads/2019/09/%E0%B8%9B%E0%B8%81_Rehab-Med-Curriculum-Revised-2561_March-20-2019_Final-OK.pdf.
The Board of Training and Examination in Rehabilitation Medicine The Royal College of Physiatrists of Thailand. Entrustable Professional Activities (EPAs) and Workplace-based Assessment (WPBA) in Rehabilitation Medicine Residency Training [Internet]; 2020 [updated 2020; cited 2023 Feb 2] Available from: http://rehabmed.or.th/main/wp-content/uploads/2020/09/EPAs-and-WPBA_Proof-IV_July-15-2020_Final-for-print.pdf.
Nasca TJ, Philibert I, Brigham T, Flynn TC. The Next GME Accreditation System — Rationale and Benefits. New England Journal of Medicine. 2012;366(11):1051-6.
Carraccio C, Iobst WF, Philibert I. Milestones: Not Millstones but Stepping Stones. Journal of graduate medical education. 2014;6(3):589-90.
Cook DA, Artino AR, Jr. Motivation to learn: an overview of contemporary theories. Med Educ. 2016;50(10):997-1014.
The Board of Training and Examination in Rehabilitation Medicine The Royal College of Physiatrists of Thailand. Entrustable Professional Activities (EPAs) and Workplace-based Assessment (WPBA) in Rehabilitation Medicine Residency Training [Internet]; 2021 [updated 2021; cited 2023 Feb 2] Available from: https://www.rehabmed.or.th/main/wp-content/uploads/2021/07/Final_EPA_WPBA_2021-Revision-1.pdf.
Chatterjee D, Corral J. How to Write Well-Defined Learning Objectives. J Educ Perioper Med. 2017;19(4):E610.
Heinich R, Molenda M, Russell JD, Smaldino SE. Instructional Media and Technologies for Learning. 7th ed: Pearson; 2002.
Artino AR, Jr., La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36(6):463-74.
Collins NS. Motivation and Self-Regulated Learning: Theory, Research, and Applications. The Journal of Higher Education. 2009;80:476 - 9.
Kusurkar RA, Ten Cate TJ, van Asperen M, Croiset G. Motivation as an independent and a dependent variable in medical education: A review of the literature. Medical Teacher. 2011;33(5):e242-e62.
Panadero E. A Review of Self-regulated Learning: Six Models and Four Directions for Research. Front Psychol. 2017;8:422.
Zimmerman BJ, Risemberg R. Chapter 4 - Self-Regulatory Dimensions of Academic Learning and Motivation. In: Phye GD, editor. Handbook of Academic Learning. San Diego: Academic Press; 1997. p. 105-25.
Sawatsky AP, Halvorsen AJ, Daniels PR, Bonnes SL, Issa M, Ratelle JT, et al. Characteristics and quality of rotation-specific resident learning goals: a prospective study. Med Educ Online. 2020;25(1):1714198.
Nothnagle M, Anandarajah G, Goldman RE, Reis S. Struggling to Be Self-Directed: Residents' Paradoxical Beliefs About Learning. Academic Medicine. 2011;86(12):1539-44.
Colthart I, Bagnall G, Evans A, Allbutt H, Haig A, Illing J, et al. The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME Guide no. 10. Med Teach. 2008;30(2):124-45.
Brydges R, Butler D. A reflective analysis of medical education research on self-regulation in learning and practice. Medical Education. 2012;46(1):71-9.
van Houten-Schat MA, Berkhout JJ, van Dijk N, Endedijk MD, Jaarsma ADC, Diemers AD. Self-regulated learning in the clinical context: a systematic review. Med Educ. 2018;52(10):1008-15.
Brewster LP, Risucci DA, Joehl RJ, Littooy FN, Temeck BK, Blair PG, et al. Comparison of resident self-assessments with trained faculty and standardized patient assessments of clinical and technical skills in a structured educational module. Am J Surg. 2008;195(1):1-4.
Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. Jama. 2006;296(9):1094-102.
Zevin B. Self versus external assessment for technical tasks in surgery: a narrative review. J Grad Med Educ. 2012;4(4):417-24.
Blanch-Hartigan D. Medical students' self-assessment of performance: results from three meta-analyses. Patient Educ Couns. 2011;84(1):3-9.
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














