Transvaginal Urethrolysis As A Treatment Option For Women With Recurrent Cystitis
DOI:
https://doi.org/10.33192/smj.v75i5.261230Keywords:
recurrent cystitis, voiding dysfunction, bladder outlet obstruction, detrusor underactivity, urethrolysisAbstract
Objectives: To demonstrate the outcome of transvaginal urethrolysis as a treatment option for women with recurrent cystitis, which could be caused from voiding problems. In the case of a failure of non-invasive treatment, the surgical procedure to decrease outlet resistance may have a role.
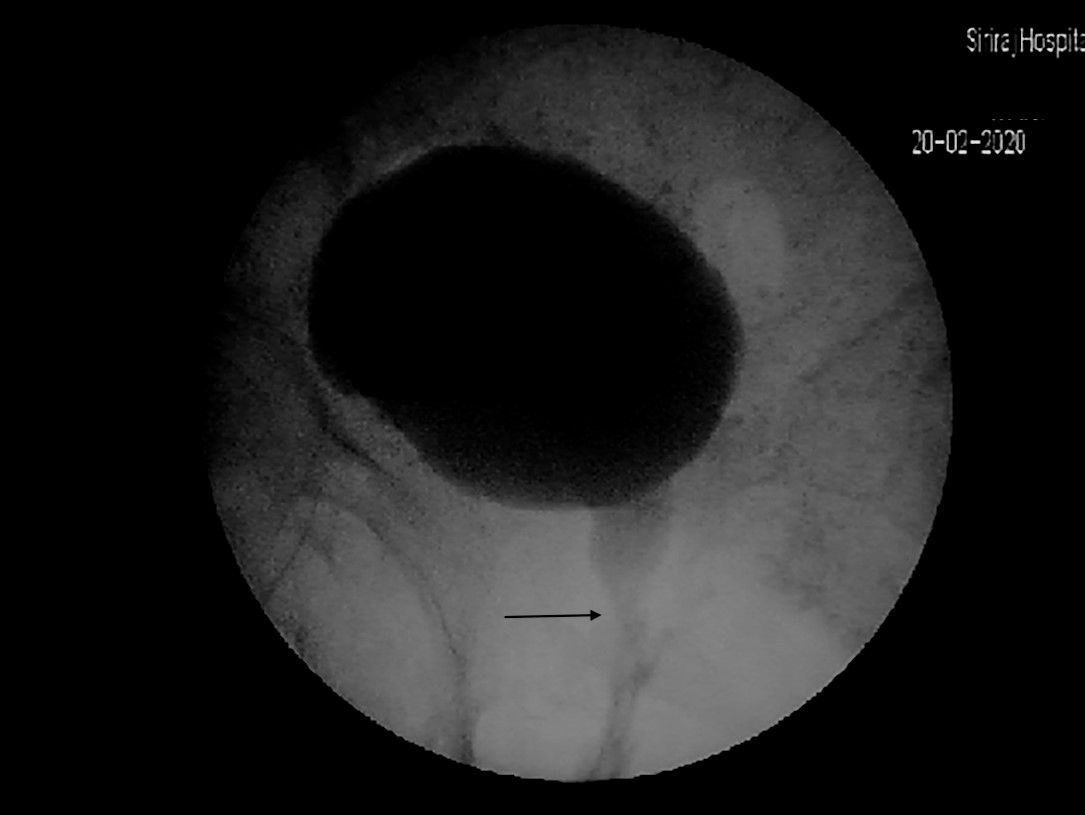
Materials and Methods: Between January 2016 and December 2020, women with recurrent cystitis who underwent urethrolysis at Siriraj Hospital were retrospectively reviewed. Only women who were followed-up for more than 6 months were analyzed. Cure was defined by no clinical symptoms of cystitis, no pyuria on urine analysis, and/or negative urine culture during the follow-up period.
Results: In total, 52 women underwent transvaginal urethrolysis. The overall cure rate was observed 53.9% (28 cases) at a median follow-up time of 11.9 (6–59) months. Eighteen of the 44 cases (40.9%) who underwent a video urodynamics study showed bladder outlet obstruction, defined as a Solomon–Greenwell bladder outlet obstruction index of more than 5. None of the characteristics or urodynamics parameters showed statistically significant differences between the cure and failure groups. Postoperative urinary incontinence was reported in 14 cases (26.9%) but showed no statistical difference between the cure and failure group (p = 0.748).
Conclusion: Bladder outlet obstruction is a common cause of recurrent cystitis. Transvaginal urethrolysis may have a role as treatment for women with recurrent cystitis from voiding dysfunction who have failed non- and less-invasive treatments. Here, the overall cure rate was 53.8%. A factor associated with the cure rate could not be demonstrated in this study.
References
Anger J, Lee U, Ackerman AL, Chou R, Chughtai B, Clemens JQ, et al. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. J Urol 2019;202(2):282-9.
Foxman B, Barlow R, D'Arcy H, Gillespie B, Sobel JD. Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol 2000;10(8):509-15.
Ikaheimo R, Siitonen A, Heiskanen T, Karkkainen U, Kuosmanen P, Lipponen P, et al., Recurrence of urinary tract infection in a primary care setting: analysis of a 1-year follow-up of 179 women. Clin Infect Dis 1996;22(1):91-9.
Foxman B. Recurring urinary tract infection: incidence and risk factors. Am J Public Health 1990;80(3):331-3.
Ruben FL, Dearwater SR, Norden CW, Kuller LH, Gartner K, Shalley A, et al., Clinical infections in the noninstitutionalized geriatric age group: methods utilized and incidence of infections. The Pittsburgh Good Health Study. Am J Epidemiol 1995;141(2):145-57.
Farrar DJ, Green NA, Ashken MH. An evaluation of Otis urethrotomy in female patients with recurrent urinary tract infections. Br J Urol 1973;45(6):610-5.
Keitzer WA, Allen JS. Operative treatment of chronic cystitis by urethrotomy: 10 years of experience. J Urol 1970;103(4):429-31.
Smith PJ, Powell PH, George NJ, Kirk D. Urethrolysis in the management of females with recurrent frequency and dysuria. Br J Urol 1981;53(6):634-6.
Minardi D, Pellegrinelli F, Conti A, Fontana D, Mattia M, Milanese G, et al. alpha1-Blockers for the treatment of recurrent urinary tract infections in women with dysfunctional voiding: a prospective randomized study. Int J Urol 2015;22(1):115-21.
Nitti VW, Raz S. Obstruction following anti-incontinence procedures: diagnosis and treatment with transvaginal urethrolysis. J Urol 1994;152(1):93-8.
McCrery R, Appell R. Transvaginal urethrolysis for obstruction after antiincontinence surgery. Int Urogynecol J Pelvic Floor Dysfunct 2007;18(6):627-33.
Foster HE, McGuire EJ. Management of urethral obstruction with transvaginal urethrolysis. J Urol 1993;150(5 Pt 1):1448-51.
Carr LK, Webster GD. Voiding dysfunction following incontinence surgery: diagnosis and treatment with retropubic or vaginal urethrolysis. J Urol 1997;157(3):821-3.
Goldman HB, Rackley RR, Appell RA. The efficacy of urethrolysis without re-suspension for iatrogenic urethral obstruction. J Urol 1999;161(1):196-8; discussion 198-9.
Solomon E, Yasmin H, Duffy M, Rashid T, Akinluyi E, Greenwell TJ. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourol Urodyn 2018;37(1):368-78.
Woodman PJ, Ruiz HL. Retropubic urethrolysis without resuspension for the management of posturethropexy urinary retention and voiding dysfunction. Mil Med 2004;169(2):117-20.
Meier K, and Padmanabhan P. Female bladder outlet obstruction: an update on diagnosis and management. Curr Opin Urol 2016;26(4):334-41.
Essenhigh DM, Ardran GM, Cope V. A study of the bladder outlet in lower urinary tract infections in women. Br J Urol 1968;40(3):268-77.
McCannel DA, Haile W. Urethral narrowing and its treatment: a possible solution for the problems of recurrent urinary infection and the "irritable bladder". Int Urol Nephrol 1982;14(4):407-14.
Immergut MA, Gilbert EC. The clinical response of women to internal urethrotomy. J Urol 1973;109(1):90-1.
Pang KH, Campi R, Arlandis S, Bo K, Chapple CR, Costantini E, et al., Diagnostic Tests for Female Bladder Outlet Obstruction: A Systematic Review from the European Association of Urology Non-neurogenic Female LUTS Guidelines Panel. Eur Urol Focus 2022;8(4):1015-30.
Giannis G, Bousouni E, Mueller MD, Imboden S, Mohr S, Raio L, et al. Can urethrolysis resolve outlet obstruction related symptoms after Burch colposuspension for stress urinary incontinence? Eur J Obstet Gynecol Reprod Biol 2015;195:103-7.
Starkman JS, Duffy JW 3rd, Wolter CE, Kaufman MR, Scarpero HM, Dmochowski RR. The evolution of obstruction induced overactive bladder symptoms following urethrolysis for female bladder outlet obstruction. J Urol 2008;179(3):1018-23.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














