The Relationship between Kolb Learning Style and Academic Performances in Orthopedic Residents
DOI:
https://doi.org/10.33192/smj.v75i5.261255Keywords:
Kolb learning styles, Orthopedic residents, academic performanceAbstract
Objective: The assimilating and converging Kolb learning style were reported to have positive correlation with critical thinking ability in Orthopedic resident. However, the relationship between Kolb learning styles and academic performance remained controversy. The objective of this study is to report the relationship between Kolb learning style and academic performance in Orthopedic residents.
Materials and Methods: The causal comparative cross-sectional study on 48 Orthopedic residents of academic year 2020 was conducted. The demographic characteristics of the participants were reviewed. The scores from the multiple choices question (MCQ) in-training examination, the objective structured clinical examination (OSCE) and the global performance rating scale were collected to represent academic performances of each Miller’s pyramid of assessment level. The Kolb learning style inventory were allocated. The statistical analysis was performed and p < 0.05 was considered statistically significant difference.
Results: The response rate was 100%. There was no statistically significant difference of MCQ in-training examination, OSCE and global performance rating scale among each learning style as p=0.789, 0.493 and 0.407, respectively. The assimilating and converging styles were the 2 learning styles which had the academic performance scores above the average scores in all assessments.
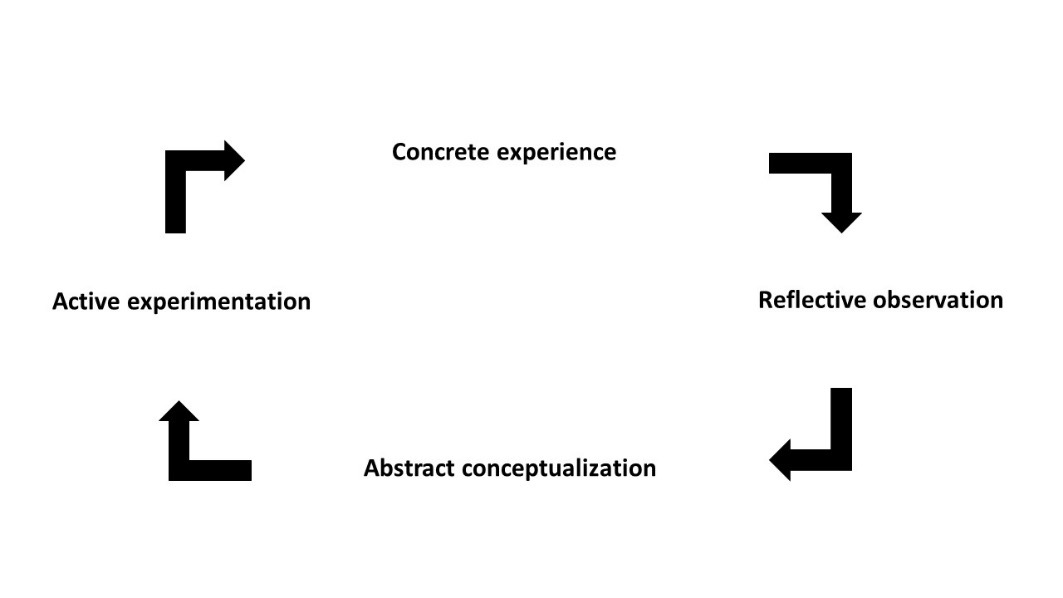
Conclusion: This study could not demonstrate the significant difference of academic performances among Kolb learning style in Orthopedic residents. However, the assimilating and converging style had the consistent scores above average scores in all domains. The Orthopedic learning experience should focus on the development of reflective observation, abstract conceptualization and active experimentation to facilitate effective improvement in academic performance of the residents.
References
Richard RD, Deegan BF, Klena JC. The Learning Styles of Orthopedic Residents, Faculty and Applicants at an Academic Program. J Surg Educ. 2014;71(1):110-8.
Harnroongroj T, Thanapipatsiri S, Nopparatjamjomras TN, Iramaneerat C. The Relationship Between Learning Styles, Academic Achievement, and Critical Thinking Skills Among Orthopedic Residents. Proceeding of Graduate Research Forum. 2022
Sand JN, Elison-Bowers P, Wing II TJ, Kendrick L. Experiential Learning and Clinical Education. Psychology. 2014;18(4):1-7.
Kolb DA. Experiential learning: Experience as the source of learning and development. Englewood Cliffs. New Jersey. Prentice-Hall; 1984.
McCarthy M. Experiential Learning Theory: From Theory to Practice. Journal of Business & Economics Research. 2016;14(3):91-100.
Lerdlop W. Learning Styles of Students in the Faculty of Science and Technology. Suan Sunandha Rajabhat University, Bangkok. Bangkok: Suan Sunandha Rajabhat University; 2011.
Kolb AY, Kolb DA. The Kolb Learning Style Inventory Version 3.1 2005 Technical Specifications. Experiential Based Learning Systems [Internet]. 2005
[Cited 2022 November 30]. Available from: http://www.learningfromexperience.com/.
Hayat AA, Shateri K, Amini M, Shokrpour N. Relationships between academic self-efficacy, learning-related emotions, and metacognitive learning strategies with academic performance in medical students: a structural equation model. BMC Med Educ. 2020;20:76.
Piumatti G, Guttormsen S, Zurbuchen B, Abbiati M, Gerbase MW, Baroffio A. Trajectories of learning approaches during a full medical curriculum: impact on clinical learning outcomes. BMC Med Educ. 2021;21:370.
Kusurka RA, Croiset G, Galindo-Garre F, Ten Cate O. Motivational profiles of medical students: Association with study effort, academic performance and exhaustion. BMC Med Educ. 2013;13:87.
Quillin RC, Cortez AR, Pritts TA, Hanseman DJ, Edwards MJ, Davis BR. Surgical resident learning styles have changed with work hours. J Surg Res. 2016;200:39-45. Mamede S, Schmidt HG. Reflection in Medical Diagnosis: A Literature Review. Health Professional Education. 2017;3:15-25.
Mamede S, van Gog T, Moura AS, de Faria RM, Peixoto JM, Rikers RM, Schmidt HG. Reflection as a strategy to foster medical students' acquisition of diagnostic competence. Med Educ. 2012;46(5):464-72.
Hatton N, Smith D. Reflection in teacher education: Towards definition and implementation. Teaching and Teacher Education. 1995;11(1):33-49.
Robertson K. Reflection in professional practice and education. Aust Fam Physician. 2005;34(9):781-3.
Branch WT, Paranjape A. Feedback and reflection: teaching methods for clinical settings. Acad Med. 2002;77:1185-8.
Yari SS, Jandhyala CK, Sharareh B, Athiviraham A, Shybut TB. Efficacy of a virtual arthroscopic simulator for Orthopaedic surgery residents by year in training. Orthop J Sports Med. 2018;6(11):2325967118810176.
Aim F, Lonjon G, Hannouche D, Nizard R. Effectiveness of virtual reality training in Orthopaedic surgery. Arthroscopy. 2016;32(1):224-32.
Julthongpipat K, Dumavibhat C, Towashiraporn K, Patpituck P. Development of Simulation Model for Transradial Catheterization Practice for Physicians. Siriraj Med J. 2022;74(9):570-4.
Angelo RL, Ryu RKN, Pedowitz RA, Beach W, Burns J, Dodds J, et al. A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy. 2015;31(10):1854-71.
Wadey DM, Dev P, Buckley R, Walker D, Hedden D. Competencies for Canadian Orthopaedics surgery core curriculum. J Bone Joint Surg Br. 2009;91(12):1618-22.
Dwyer T, Wadey V, Archibald D, Kraemer W, Shantz JS, Townley J, et al. Cognitive and psychomotor entrustable professional activities: Can simulators help assess competency in trainees. Clin Orthop Relat Res. 2016;474:926-34.
Van Loon KA, Driessen EW, Teunissen PW, Scheele F. Experiences with EPAs, potential benefits and pitfalls. Medical Teacher. 2014;36(8):698-702.
Pinilla S, Lenouvel E, Cantisani A, Kloppel S, Strik W, Huwendiek S, et al. Working with entrustable professional activities in clinical education in undergraduate medical education: a scoping review. BMC Med Educ. 2021;21:172.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














