Pathological and Oncologic Outcomes of Consolidation Chemotherapy in Locally Advanced Rectal Cancer after Neoadjuvant Chemoradiation
DOI:
https://doi.org/10.33192/smj.v75i4.261259Keywords:
Consolidation, induction chemotherapy, total neoadjuvant therapy, rectal cancer, pathologic complete responseAbstract
Objective: The current standard of care for locally advanced rectal cancer is associated with multimodality therapy. Neoadjuvant chemoradiation significantly decreased the locoregional recurrence rate and improved survival. However, distant metastasis develops rather than local recurrence, which becomes the leading cause of death. This study aimed to evaluate the oncological outcomes of total neoadjuvant therapy (TNT) in locally advanced rectal cancer.
Materials and Methods: This retrospective study recruited 18 patients diagnosed with locally advanced rectal adenocarcinoma (cT3-4 or cN1-2), treated with consolidation TNT. The primary endpoint was pathological complete response (pCR). The secondary endpoint included postoperative outcomes, local recurrences, and distant metastases.
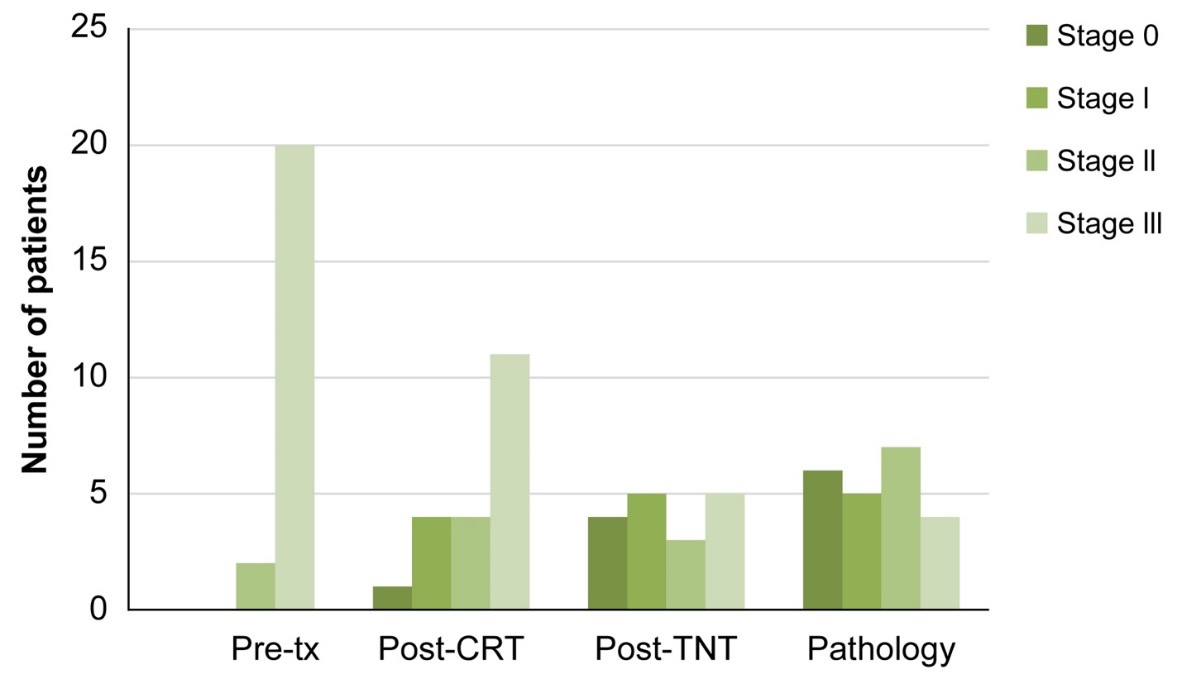
Results: The pathologic complete response was observed in 27.8% of consolidation therapy cases. Downstaging of the T-category was achieved in 10 (55.6%) patients, and downstaging of the N-category was achieved in 14 (77.8%) patients. Only one patient who achieved pCR developed distant metastasis, whereas all patients with pathological stage III developed distant metastasis.
Conclusions: TNT is a promising approach for patients with locally advanced rectal cancer. This strategy improved complete pathologic response rates in TNT, and pCR was found to be associated with fewer local recurrences and greater disease-free survival.
References
Lohsiriwat V, Chaisomboon N, Pattana-Arun J. Current colorectal cancer in Thailand. Ann Coloproctol 2020; 36: 78–82.
Techawathanawanna S, Nimmannit A, Akewanlop C. Clinical characteristics and disease outcome of UICC stages I-III colorectal cancer patients at Siriraj Hospital. J Med Assoc Thai 2012; 95:S189–S198.
Sauer R, Liersch T, Merkel S, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol 2012; 30: 1926–1933.
Peeters KC, Marijnen CA, Nagtegaal ID, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 2007; 246: 693–701.
Glynne-Jones R, Wyrwicz L, Tiret E, et al. Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018; 29: iv263.
Bosset JF, Calais G, Mineur L, et al. Fluorouracil-based adjuvant chemotherapy after preoperative chemoradiotherapy in rectal cancer: long-term results of the EORTC 22921 randomised study. Lancet Oncol 2014; 15: 184–190.
Franke AJ, Parekh H, Starr JS, et al. Total neoadjuvant therapy: a shifting paradigm in locally advanced rectal cancer management. Clin Colorectal Cancer 2018; 17: 1–12.
Kasi A, Abbasi S, Handa S, et al. Total neoadjuvant therapy vs standard therapy in locally advanced rectal cancer: a systematic review and meta-analysis. JAMA Netw Open 2020; 3: e2030097.
Kong JC, Soucisse M, Michael M, et al. Total neoadjuvant therapy in locally advanced rectal cancer: a systematic review and metaanalysis of oncological and operative outcomes. Ann Surg Oncol 2021; 28: 7476–7486.
Liu S, Jiang T, Xiao L, et al. Total neoadjuvant therapy (TNT) versus standard neoadjuvant chemoradiotherapy for locally advanced rectal cancer: a systematic review and meta-analysis. Oncologist 2021; 26: e1555–e1566.
Amin MB, Greene FL, Edge SB, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin 2017; 67: 93–99.
Trakarnsanga A, Gonen M, Shia J, et al. Comparison of tumor regression grade systems for locally advanced rectal cancer after multimodality treatment. J Natl Cancer Inst 2014; 106.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187–196.
Trakarnsanga A, Ithimakin S, Weiser MR. Treatment of locally advanced rectal cancer: controversies and questions. World J Gastroenterol 2012; 18: 5521–5532.
Rodel C, Graeven U, Fietkau R, et al. Oxaliplatin added to fluorouracil-based preoperative chemoradiotherapy and postoperative chemotherapy of locally advanced rectal cancer (the German CAO/ARO/AIO-04 study): final results of the multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 2015; 16: 979–989.
Garcia-Aguilar J, Hernandez de Anda E, Sirivongs P, et al. A pathologic complete response to preoperative chemoradiation is associated with lower local recurrence and improved survival in rectal cancer patients treated by mesorectal excision. Dis Colon Rectum 2003; 46: 298–304.
Martin ST, Heneghan HM, Winter DC. Systematic review and meta-analysis of outcomes following pathological complete response to neoadjuvant chemoradiotherapy for rectal cancer. Br J Surg 2012; 99: 918–928.
Petrelli F, Trevisan F, Cabiddu M, et al. Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg 2020; 271: 440–448.
Fokas E, Schlenska-Lange A, Polat B, et al. Chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for patients with locally advanced rectal cancer: long-term results of the CAO/ARO/AIO-12 randomized clinical trial. JAMA Oncol 2022; 8: e215445.
Cui J, Fang H, Zhang L, et al. Advances for achieving a pathological complete response for rectal cancer after neoadjuvant therapy. Chronic Dis Transl Med 2016; 2: 10–16.
Garcia-Aguilar J, Smith DD, Avila K, et al. Optimal timing of surgery after chemoradiation for advanced rectal cancer: preliminary results of a multicenter, nonrandomized phase II prospective trial. Ann Surg 2011; 254: 97–102.
Bahadoer RR, Dijkstra EA, van Etten B, et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol 2021; 22: 29–42.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














