Comparative Effectiveness of Video and Face-to- Face Sessions to Educate Hospitalized Patients on Cancer Pain Management
DOI:
https://doi.org/10.33192/smj.v75i4.261563Keywords:
Cancer pain, Hospitalization, Humans, Neoplasm, Pain management, Patient education, Randomized controlled trialAbstract
Objective: Patients’ lack of knowledge of cancer pain management affects pain outcomes. This study compared the effectiveness of cancer pain management achieved in a previous retrospective study (“P-group”), in which hospitalized cancer pain individuals received no pain education, with the pain management achieved by 2 study groups. One group received pain management information via video sessions (“V-group”) and the other via face-to-face coaching (“F-group”). The study’s secondary aims were to compare the 2 interventions’ psychological, quality-of-life, and opioid-consumption impacts.
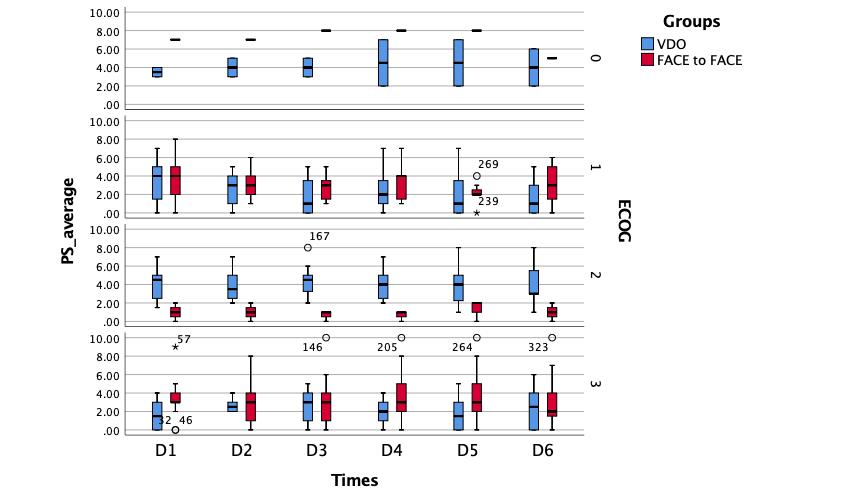
Materials and Methods: This single-blinded, randomized, controlled trial enrolled hospitalized cancer pain patients aged between 18 and 70 with an Eastern Clinical Oncology Group performance status < 4. They were assigned to V- and F-groups to receive information on managing cancer pain. “Successful pain control” was defined as “no to mild pain” or a numerical rating scale score < 4 on Day 6. Pain intensity and opioid consumption (morphine-equivalent daily dosage) were recorded daily from baseline to Day 6. Psychological status (Hospital Anxiety and Depression Scale) and quality of life (Functional Assessment of Cancer Therapy–General) were assessed at baseline and Day 6.
Results: Fifty-nine participants were analyzed (V-group: 31; F-group: 28). Both groups had significantly higher successful pain outcomes than the P-group (P < .001). The V- and F-groups had no significant differences in successful pain control (20 [65%] vs 19 [68%]; P = .787), psychological effects, quality of life, or opioid consumption.
Conclusions: Video sessions are an alternative means of educating hospitalized cancer pain patients and reducing healthcare providers’ workloads.
References
Wangnamthip S, Euasobhon P, Siriussawakul A, Jirachaipitak S, Laurujisawat J, Vimolwattanasarn K. Effective pain management for inpatients at Siriraj hospital: a retrospective study. J Med Assoc Thai. 2016;99(5):565-71.
Paice JA. Pain in Cancer Survivors: How to Manage. Curr Treat Options Oncol. 2019;20(6):48.
Organization WH. WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. 2018.
Bouhassira D, Luporsi E, Krakowski I. Prevalence and incidence of chronic pain with or without neuropathic characteristics in patients with cancer. PAIN. 2017;158(6):1118-25.
van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on Prevalence of Pain in Patients With Cancer: Systematic Review and Meta-Analysis. J Pain Symptom Manage. 2016;51(6):1070-90 e9.
Wangnamthip S. Cancer Pain Management: Is It Still Problematic? Siriraj Medical Journal. 2019;71(1).
Seangrung R, Ahuja M, Pasutharnchat K, Mahawan R. Factors influencing non-adherence to opioids in cancer patients: a mixed-methods cross-sectional study. F1000Res. 2020;9:1471.
Bennett MI, Bagnall AM, Jose Closs S. How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta-analysis. Pain. 2009;143(3):192-9.
National Comprehensive Cancer Network, NCCN Clinical Practice Guidelines in Oncology: Adult Cancer Pain, Version 3.2019.
Bennett MI, Eisenberg E, Ahmedzai SH, Bhaskar A, O’Brien T, Mercadante S, et al. Standards for the management of cancer-related pain across Europe-A position paper from the EFIC Task Force on Cancer Pain. Eur J Pain. 2019;23(4):660-8.
Koh SJ, Keam B, Hyun MK, Ju Seo J, Uk Park K, Oh SY, et al. Cancer Pain Management Education Rectifies Patients’ Misconceptions of Cancer Pain, Reduces Pain, and Improves Quality of Life. Pain Med. 2018;19(12):2546-55.
ElMokhallalati Y, Mulvey MR, Bennett MI. Interventions to support self-management in cancer pain. Pain Rep. 2018;3(6):e690.
Martin MY, Pisu M, Kvale EA, Johns SA. Developing effective cancer pain education programs. Curr Pain Headache Rep. 2012;16(4):332-42.
Oldenmenger WH, Geerling JI, Mostovaya I, Vissers KCP, de Graeff A, Reyners AKL, et al. A systematic review of the effectiveness of patient-based educational interventions to improve cancer-related pain. Cancer Treat Rev. 2018;63:96-103.
Treillet E, Laurent S, Hadjiat Y. Practical management of opioid rotation and equianalgesia. Journal of pain research. 2018:2587-601.
Datta SS, Ghosal N, Daruvala R, Chakraborty S, Shrimali RK, van Zanten C, et al. How do clinicians rate patient’s performance status using the ECOG performance scale? A mixed-methods exploration of variability in decision-making in oncology. Ecancermedicalscience. 2019;13:913.
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17-24.
Nilchaikovit T. Development of Thai version of hospital anxiety and depression scale in cancer patients. J Psychiatr Assoc Thai. 1996;4:18-30.
Thanasilp S, Suwannapong K, Long NH. Validation of the Thai Version of the Functional Assessment of Cancer Therapy-General (FACT-G) for Persons with Terminal Cancer. Journal of Pain and Symptom Management. 2018;56(6):e137-e8.
Almasri BM, McDonald DD. Barriers and Facilitators of Pain Self-Management Among Patients with Cancer: An Integrative Review. Pain Manag Nurs. 2023.
Bashayreh A. Opioidphobia and Cancer Pain Management. Journal of Pediatric Hematology Oncology. 2011;33:60-1.
Lam M, Choi M, Lam HR, Agarwal A, Chow R, Chow S, et al. Use of multimedia in patient and caregiver education for cancer pain management: a literature review. Annals of Palliative Medicine. 2017;6:66-72.
Information Hr. Statistics of the number of medical personnel in Thailand in National Statistical Office 2022.
Harbitza MB, Stenslandb PS, Gaskic M. Rural general practice staff experiences of patient safety incidents and low quality of care in Norway: an interview study. Family Practice. 2022;39:130-6.
Daurat A, Boudet E, Daurat G, Roger C, Gris J-C, Tunez V, et al. Evaluation of the non-compliance with grouping guidelines which may lead to “wrong blood in tube”: an observational study and risk factor analysis. Transfusion Clinique et Biologique. 2017;24(2):47-51.
Karadzinska-Bislimovska J, Basarovska V, Mijakoski D, Minov J, Stoleski S, Angeleska N, et al. Linkages between workplace stressors and quality of care from health professionals’ perspective - Macedonian experience. British Journal of Health Psychology. 2014;19(2).
Silapavitayatorn B, Chitpakdee B. The Use of Health Information Technology in Nursing for Patient Safety. Journal of Nursing and Health Care. 2020;38(2):6-14.
Jagota P, Jongsuntisuk P, Plengsri R, Chokpatcharavate M, Phokaewvarangkul O, Chirapravati V, et al. If Your Patients Were Too Embarrassed to Go Out in Public, What Would You Do? - Public Education to Break the Stigma on Parkinson’s Disease Using Integrated Media. Patient Related Outcome Measures 2020;11:143-8.
Thomas ML, Fahey KF, Christine Miaskowski R, editors. A randomized, clinical trial of education or motivational-interviewing-based coaching compared to usual care to improve cancer pain management. Oncology Nursing Forum; 2012: Oncology Nursing Society.
Syrjala KL, Abrams JR, Polissar NL, Hansberry J, Robison J, DuPen S, et al. Patient training in cancer pain management using integrated print and video materials: a multisite randomized controlled trial. PAIN. 2008;135(1-2):175-86.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














