Social Support in Quality of Life among Breast Cancer Patients after Diagnosis: A Bibliometric Analysis
DOI:
https://doi.org/10.33192/smj.v75i7.261979Keywords:
Breast cancer, bibliometric analysis, Social Support, quality of life, journal, ScopusAbstract
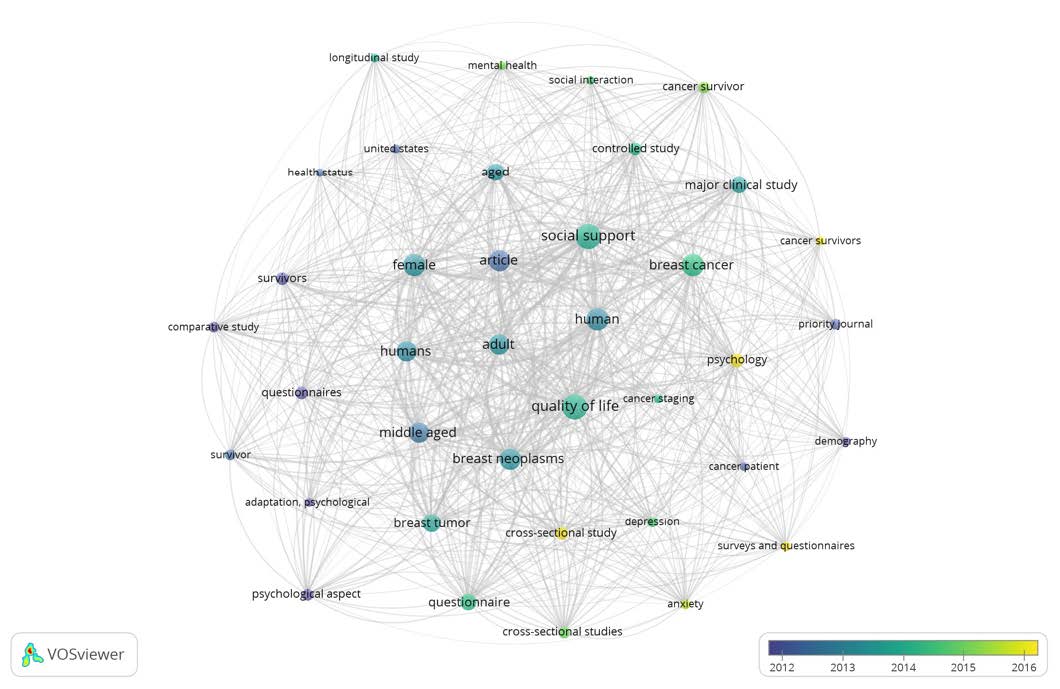
In terms of bibliometric analysis, there are no studies related to the impact of social support on breast cancer survivors' quality of life. Therefore, this study aims to provide a bibliometric assessment of results on social support in quality of life in breast cancer patients. The studies for the dataset were selected from Scopus published in the year 2001–2021 based on their relevancy to the established subjects. The VOSviewer software was used for bibliometric analysis to represent the performance of publications covering annual outputs, mainstream journals leading countries, institutions, research tendencies, and hotspots. The analysis of the findings indicated only 45 articles over the range of 2001-2021. The highest number of publications was published in 2021, and the lowest was in 2002-2004 and 2006. Social support strongly correlates with the psychological adjustment of adherence to cancer treatment. Only one study failed to find an association between social support and suicide after a cancer diagnosis. Meanwhile, China, the United States, and Hong Kong contributed to social support. Instrumental, financial, information, and emotional support were reported as domains needed to support breast cancer patients. This bibliometric analysis provides the results of thoughts and insights about the development needed by breast cancer patients to prolong survival.
References
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2020). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 0(2020), 1–41. https://doi.org/10.3322/caac.21660
Momenimovahed, Z., & Salehiniya, H. (2019). Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer : Targets and Therapy, 11(2019), 151–164. https://doi.org/10.2147/BCTT.S176070
Thun, M. J., DeLancey, J. O., Center, M. M., Jemal, A., & Ward, E. M. (2010). The global burden of cancer: priorities for prevention. Carcinogenesis, 31(1), 100–110. https://doi.org/10.1093/carcin/bgp263
Arthur, R. S., Wang, T., Xue, X., Kamensky, V., & Rohan, T. E. (2020). Genetic Factors, Adherence to Healthy Lifestyle Behavior, and Risk of Invasive Breast Cancer Among Women in the UK Biobank. Journal of the National Cancer Institute, 112(9), 893–901. https://doi.org/10.1093/jnci/djz241
Lofterød, T., Frydenberg, H., Flote, V., Eggen, A. E., McTiernan, A., Mortensen, E. S., … Thune, I. (2020). Exploring the effects of lifestyle on breast cancer risk, age at diagnosis, and survival: the EBBA-Life study. Breast Cancer Research and Treatment, 182(1), 215–227. https://doi.org/10.1007/s10549-020-05679-2
Chen, H. H. W., & Kuo, M. T. (2017). Improving radiotherapy in cancer treatment: Promises and challenges. Oncotarget, 8(37), 62742–62758. https://doi.org/10.18632/oncotarget.18409
Chudasama, R., Fenton, M. A., & Dizon, D. S. (2020). Guidelines of Chinese Society of Clinical Oncology (CSCO) on Diagnosis and Treatment of Breast Cancer: an appraisal. Translational Breast Cancer Research, 1(2020), 24–24. https://doi.org/10.21037/tbcr-2020-3
Glynne-Jones, R., Wyrwicz, L., Tiret, E., Brown, G., Rödel, C., Cervantes, A., … ESMO Guidelines Committee. (2017). Rectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 28(suppl_4), iv22–iv40. https://doi.org/10.1093/annonc/mdx224
Moo, T.-A., Sanford, R., Dang, C., & Morrow, M. (2018). Overview of Breast Cancer Therapy. PET clinics, 13(3), 339–354. https://doi.org/10.1016/j.cpet.2018.02.006
Postmus, P. E., Kerr, K. M., Oudkerk, M., Senan, S., Waller, D. A., Vansteenkiste, J., … ESMO Guidelines Committee. (2017). Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 28(suppl_4), iv1–iv21. https://doi.org/10.1093/annonc/mdx222
Tong, C. W. S., Wu, M., Cho, W. C. S., & To, K. K. W. (2018). Recent Advances in the Treatment of Breast Cancer. Frontiers in Oncology, 8(2018), 227. https://doi.org/10.3389/fonc.2018.00227
Bartlett, J. M. S., Sgroi, D. C., Treuner, K., Zhang, Y., Ahmed, I., Piper, T., … Rea, D. W. (2019). Breast Cancer Index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the Adjuvant Tamoxifen—To Offer More? (aTTom) trial. Annals of Oncology, 30(11), 1776–1783. https://doi.org/10.1093/annonc/mdz289
Burstein, H. J., Curigliano, G., Loibl, S., Dubsky, P., Gnant, M., Poortmans, P., … Thurlimann, B. (2019). Estimating the benefits of therapy for early-stage breast cancer: the St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Annals of Oncology, 30(10), 1541–1557. https://doi.org/10.1093/annonc/mdz235
McFarland, D. C., Shaffer, K. M., Tiersten, A., & Holland, J. (2018). Prevalence of Physical Problems Detected by the Distress Thermometer and Problem List in Patients with Breast Cancer. Psycho-oncology, 27(5), 1394–1403. https://doi.org/10.1002/pon.4631
Roguski, A., Rayment, D., Whone, A. L., Jones, M. W., & Rolinski, M. (2020). A Neurologist’s Guide to REM Sleep Behavior Disorder. Frontiers in Neurology, 11(2020), 610. https://doi.org/10.3389/fneur.2020.00610
Mogavero, M. P., DelRosso, L. M., Fanfulla, F., Bruni, O., & Ferri, R. (2021). Sleep disorders and cancer: State of the art and future perspectives. Sleep Medicine Reviews, 56(2021), 101409. https://doi.org/10.1016/j.smrv.2020.101409
Vin-Raviv, N., Akinyemiju, T. F., Galea, S., & Bovbjerg, D. H. (2018). Sleep disorder diagnoses and clinical outcomes among hospitalized breast cancer patients: a nationwide inpatient sample study. Supportive Care in Cancer, 26(6), 1833–1840. https://doi.org/10.1007/s00520-017-4012-1
Bahceli, P. Z., Arslan, S., & Ilik, Y. (2022). The effect of slow-stroke back massage on chemotherapy-related fatigue in women with breast cancer: An assessor blinded, parallel group, randomized control trial. Complementary Therapies in Clinical Practice, 46(2022), 101518. https://doi.org/10.1016/j.ctcp.2021.101518
Gong, Y., Tan, Q., Qin, Q., & Wei, C. (2020). Prevalence of postmastectomy pain syndrome and associated risk factors: A large single-institution cohort study. Medicine, 99(20), e19834. https://doi.org/10.1097/MD.0000000000019834
Liu, H., Ma, L., Li, C., Cao, B., Jiang, Y., Han, L., … Zhang, D. (2021). The molecular mechanism of chronic stress affecting the occurrence and development of breast cancer and potential drug therapy. Translational Oncology, 15(1), 101281. https://doi.org/10.1016/j.tranon.2021.101281
Finck, C., Barradas, S., Zenger, M., & Hinz, A. (2018). Quality of life in breast cancer patients: Associations with optimism and social support. International Journal of Clinical and Health Psychology : IJCHP, 18(1), 27–34. https://doi.org/10.1016/j.ijchp.2017.11.002
Finck, C., Barradas, S., Zenger, M., & Hinz, A. (2018). Calidad de vida en pacientes con cáncer de mama: asociación con optimismo y apoyo social. International Journal of Clinical and Health Psychology, 18(1), 27–34. https://doi.org/10.1016/j.ijchp.2017.11.002
Schou-Bredal, I., Heir, T., Skogstad, L., Bonsaksen, T., Lerdal, A., Grimholt, T., & Ekeberg, Ø. (2017). Datos normativos del Test de Orientación Vital Revisado (LOT-R) basados en la población. International Journal of Clinical and Health Psychology, 17(3), 216–224. https://doi.org/10.1016/j.ijchp.2017.07.005
Tian, X., Jin, Y., Chen, H., Tang, L., & Jiménez-Herrera, M. F. (2021). Relationships among social support, coping style, perceived stress, and psychological distress in chinese lung cancer patients. Asia-Pacific Journal of Oncology Nursing, 8(2), 172–179. https://doi.org/10.4103/apjon.apjon-59-20
Benson, R. B., Cobbold, B., Opoku Boamah, E., Akuoko, C. P., & Boateng, D. (2020). Challenges, Coping Strategies, and Social Support among Breast Cancer Patients in Ghana. Advances in Public Health, 2020. https://doi.org/10.1155/2020/4817932
Eom, C.-S., Shin, D. W., Kim, S. Y., Yang, H. K., Jo, H. S., Kweon, S. S., … Park, J.-H. (2013). Impact of perceived social support on the mental health and health-related quality of life in cancer patients: results from a nationwide, multicenter survey in South Korea. Psycho-Oncology, 22(6), 1283–1290. https://doi.org/10.1002/pon.3133
Nayak, M. G., George, A., Shashidhara, Y., & Nayak, B. S. (2019). Symptom Interference and Relation between the Domains of Quality of Life among Cancer Patients of Tertiary Care Hospital. Indian Journal of Palliative Care, 25(4), 575–579. https://doi.org/10.4103/IJPC.IJPC_139_19
Applebaum, A. J., Stein, E. M., Lord-Bessen, J., Pessin, H., Rosenfeld, B., & Breitbart, W. (2014). Optimism, Social Support, and Mental Health Outcomes in Patients with Advanced Cancer. Psycho-oncology, 23(3), 299–306. https://doi.org/10.1002/pon.3418
Kroenke, C. H., Kwan, M. L., Neugut, A. I., Ergas, I. J., Wright, J. D., Caan, B. J., … Kushi, L. H. (2013). Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast cancer research and treatment, 139(2), 515–527. https://doi.org/10.1007/s10549-013-2477-2
Nipp, R. D., El-Jawahri, A., Fishbein, J. N., Eusebio, J., Stagl, J. M., Gallagher, E. R., … Temel, J. S. (2016). The Relationship Between Coping Strategies, Quality of Life, and Mood in Patients with Incurable Cancer. Cancer, 122(13), 2110–2116. https://doi.org/10.1002/cncr.30025
Adam, A., & Koranteng, F. (2020). Availability, accessibility, and impact of social support on breast cancer treatment among breast cancer patients in Kumasi, Ghana: A qualitative study. PLOS ONE, 15(4), e0231691. https://doi.org/10.1371/journal.pone.0231691
Celik, G. K., Çakır, H., & Kut, E. (2021). Mediating Role of Social Support in Resilience and Quality of Life in Patients with Breast Cancer: Structural Equation Model Analysis. Asia-Pacific Journal of Oncology Nursing, 8(1), 86–93. https://doi.org/10.4103/apjon.apjon_44_20
Diem, A., & Wolter, S. C. (2013). The Use of Bibliometrics to Measure Research Performance in Education Sciences. Research in Higher Education, 54(1), 86–114. https://doi.org/10.1007/s11162-012-9264-5
Zou, X., Yue, W. L., & Vu, H. L. (2018). Visualization and analysis of mapping knowledge domain of road safety studies. Accident Analysis & Prevention, 118(2018), 131–145. https://doi.org/10.1016/j.aap.2018.06.010
Donthu, N., Kumar, S., Pandey, N., & Lim, W. M. (2021). Research Constituents, Intellectual Structure, and Collaboration Patterns in Journal of International Marketing : An Analytical Retrospective. Journal of International Marketing, 29(2), 1–25. https://doi.org/10.1177/1069031X211004234
Bornmann, L., Wagner, C., & Leydesdorff, L. (2015). BRICS countries and scientific excellence: A bibliometric analysis of most frequently cited papers. Journal of the Association for Information Science and Technology, 66(7), 1507–1513. https://doi.org/10.1002/asi.23333
van Eck, N. J., & Waltman, L. (2010). Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics, 84(2), 523–538. https://doi.org/10.1007/s11192-009-0146-3
Habibullah, G., Gul, R., Cassum, S., & Elahi, R. (2018). Experiences of the Breast Cancer Patients Undergoing Radiotherapy at a Public Hospital Peshawar Pakistan. Asia-Pacific Journal of Oncology Nursing, 5(2), 184–194. https://doi.org/10.4103/apjon.apjon_70_17
Jindal, V., Patwari, A., Bhatlapenumarthi, V., & Siddiqui, A. D. (2019). Pancytopenia: A Rare and Unusual Initial Presentation of Breast Cancer. Cureus, 11(3), e4235. https://doi.org/10.7759/cureus.4235
Harvey, J., Dittus, K., & Mench, E. (2017). eHealth and behavioral weight loss interventions for female cancer survivors: A review. Women’s Health, 13(3), 80–88. https://doi.org/10.1177/1745505717731012
Di Giacomo, D., Ranieri, J., Perilli, E., Cannita, K., Passafiume, D., & Ficorella, C. (2019). Psychological impact of clinical treatment after breast cancer diagnosis in younger patients (38–50 age range): An explorative 3-year observational study. Neurology, Psychiatry and Brain Research, 32, 85–90. https://doi.org/10.1016/j.npbr.2019.05.001
Essue, B. M., Iragorri, N., Fitzgerald, N., & de Oliveira, C. (2020). The psychosocial cost burden of cancer: A systematic literature review. Psycho-Oncology, 29(11), 1746–1760. https://doi.org/10.1002/pon.5516
Numprasit, W., Samarnthai, N., & Srianuchat, T. (2021). Pure Flat Epithelial Atypia of the Breast on Core Needle Biopsy: No Need for Surgical Excision. Siriraj Medical Journal, 73(11), 727–731.
Usta, Y. Y. (2012). Importance of social support in cancer patients. Asian Pacific journal of cancer prevention, 13(8), 3569–3572. https://doi.org/10.7314/apjcp.2012.13.8.3569
Luszczynska, A., Pawlowska, I., Cieslak, R., Knoll, N., & Scholz, U. (2013). Social support and quality of life among lung cancer patients: a systematic review. Psycho-Oncology, 22(10), 2160–2168. https://doi.org/10.1002/pon.3218
Clough-Gorr, K. M., Stuck, A. E., Thwin, S. S., & Silliman, R. A. (2010). Older Breast Cancer Survivors: Geriatric Assessment Domains Are Associated With Poor Tolerance of Treatment Adverse Effects and Predict Mortality Over 7 Years of Follow-Up. Journal of Clinical Oncology, 28(3), 380–386. https://doi.org/10.1200/JCO.2009.23.5440
Hurria, A., Togawa, K., Mohile, S. G., Owusu, C., Klepin, H. D., Gross, C. P., … Tew, W. P. (2011). Predicting Chemotherapy Toxicity in Older Adults With Cancer: A Prospective Multicenter Study. Journal of Clinical Oncology, 29(25), 3457–3465. https://doi.org/10.1200/JCO.2011.34.7625
Soubeyran, P., Fonck, M., Blanc-Bisson, C., Blanc, J.-F., Ceccaldi, J., Mertens, C., … Rainfray, M. (2012). Predictors of Early Death Risk in Older Patients Treated With First-Line Chemotherapy for Cancer. Journal of Clinical Oncology, 30(15), 1829–1834. https://doi.org/10.1200/JCO.2011.35.7442
Caillet, P., Laurent, M., Bastuji-Garin, S., Liuu, E., Culine, S., Lagrange, J.-L., … Paillaud, E. (2014). Optimal management of elderly cancer patients: usefulness of the Comprehensive Geriatric Assessment. Clinical Interventions in Aging, 9(2014), 1645–1660. https://doi.org/10.2147/CIA.S57849
Brown, J. C., Harhay, M. O., & Harhay, M. N. (2015). Physical function as a prognostic biomarker among cancer survivors. British Journal of Cancer, 112(1), 194–198. https://doi.org/10.1038/bjc.2014.568
Verweij, N. M., Schiphorst, A. H. W., Pronk, A., van den Bos, F., & Hamaker, M. E. (2016). Physical performance measures for predicting outcome in cancer patients: a systematic review. Acta Oncologica, 55(12), 1386–1391. https://doi.org/10.1080/0284186X.2016.1219047
Abu-Helalah, M., Al-Hanaqta, M., Alshraideh, H., Abdulbaqi, N., & Hijazeen, J. (2014). Quality of life and psychological well-being of breast cancer survivors in Jordan. Asian Pacific journal of cancer prevention: APJCP, 15(14), 5927–5936. https://doi.org/10.7314/apjcp.2014.15.14.5927
Durá-Ferrandis, E., Mandelblatt, J. S., Clapp, J., Luta, G., Faul, L., Kimmick, G., … Hurria, A. (2017). Personality, coping, and social support as predictors of long-term quality-of-life trajectories in older breast cancer survivors: CALGB protocol 369901 (Alliance). Psycho-Oncology, 26(11), 1914–1921. https://doi.org/10.1002/pon.4404
Weiss Wiesel, T. R., Nelson, C. J., Tew, W. P., Hardt, M., Mohile, S. G., Owusu, C., … Group (CARG), O. behalf of the C. A. R. (2015). The relationship between age, anxiety, and depression in older adults with cancer. Psycho-Oncology, 24(6), 712–717. https://doi.org/10.1002/pon.3638
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














