Eating Disorders and their Relation with Emotional Disturbances among Undergraduate Students in Malaysia during COVID-19 Pandemic
DOI:
https://doi.org/10.33192/smj.v75i7.262003Keywords:
Eating disorders, psychological distress, social support, undergraduate students, MalaysiaAbstract
Objective: COVID-19 pandemic has greatly impacted several aspects of undergraduate students’ lives including significant effect on mental wellbeing, physical activity and eating habits which might increase the risk for developing eating disorders as these disorders tend to emerge at university age. This study aimed to assess the prevalence of eating disorders and their associated factors among undergraduate students.
Materials and Methods: A cross sectional study was conducted among 624 undergraduate students from three different universities in Malaysia. Eating disorders was assessed using the Malay version of the Eating Disorder Examination Questionnaire (EDE-Q) while the emotional disturbances was assessed by the Malay version of Kessler Psychological Distress Scale (K10) and perceived social support was assessed by the revised Malay version of The 8-item Multidimensional Scale of Perceived Social Support (MSPSS).
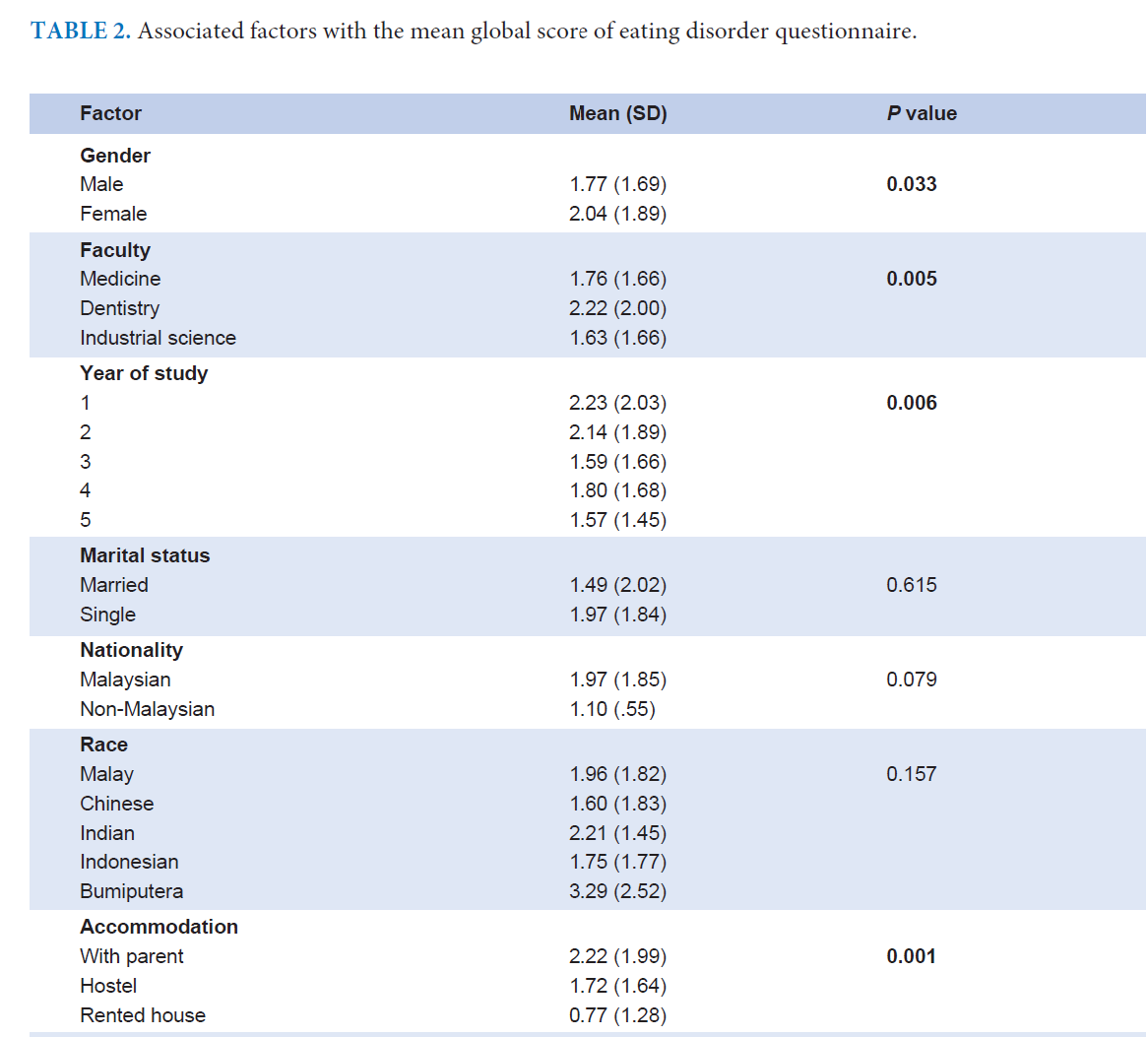
Results: The prevalence of eating disorders among students was 14.9%. There were significant differences in terms of gender and other socio-demographic factors. Eating disorders were significantly associated and positively correlated with emotional disturbances level r = 0.37. While inverse correlation between social support and eating disorders was also shown r= -0.13. Multiple linear regression analysis showed that emotional disturbances level (β = 0.212, P = 0.000) and poor social support (β = -0.126, P = 0.002) were a significantly important risk factor.
Conclusion: Eating disorders are prevalent among undergraduate students, female students, emotional disturbances and high BMI are significantly associated factors. Emotional disturbances and poor social support are predictive factor for eating disorders.
References
American Psychiatric Association. Eating disorders. December 2020. Available at: https://psychiatry.org/patients-families/eating-disorders Accessed July 2022.
Silén Y, Keski-Rahkonen A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr Opin Psychiatry. 2022;35(6):362-71.
Udo T, Grilo CM. Prevalence and correlates of DSM-5–defined eating disorders in a nationally representative sample of US adults. Biol Psychiatry. 2018;84(5):345-54.
Payton AR. Mental Health, Mental Illness, and Psychological Distress: Same Continuum or Distinct Phenomena? J Health Soc Behav. 2009;50:213-27.
Drapeau A, Marchand A, Beaulieu-Prévost D. Epidemiology of Psychological Distress, Mental Illnesses – Understanding, Prediction and Control, Prof. Luciano LAbate (Ed.), InTech, 2012.
Rasmus I, Anna‐Lisa I, Mauri M, Riittakerttu KH, Kaj B. Psychological distress and risk for eating disorders in subgroups of dieters. Eur Eat Disord Rev. 2010;18(4):296-303.
Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PloS One. 2020;15(12):e0244630.
Hossain MJ, Ahmmed F, Rahman SA, Sanam S, Emran TB, Mitra S. Impact of online education on fear of academic delay and psychological distress among university students following one year of COVID-19 outbreak in Bangladesh. Heliyon. 2021;7(6):e07388.
Rodgers RF, Lombardo C, Cerolini S, Franko DL, Omori M, Fuller‐Tyszkiewicz M, et al. The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53(7):1166-70.
Cooper M, Reilly EE, Siegel JA, Coniglio K, Sadeh-Sharvit S, Pisetsky EM, et al. Eating disorders during the COVID-19 pandemic and quarantine: an overview of risks and recommendations for treatment and early intervention. Eat Disord. 2022;30(1):54-76.
Chan YL, Samy AL, Tong WT, Islam MA, Low WY. Eating Disorder Among Malaysian University Students and Its Associated Factors. Asia Pacific Journal of Public Health. 2020;32(6-7):334-9.
Fairburn CG. Cognitive behavior therapy and eating disorders. Guilford Press; 2008.
Musa R, Bujang MA, Haniff J, Mohamad NA, Kd O, Radeef AS. Norms for Eating Disorder Examination Questionnaire (EDE-Q) among secondary school students in Kuala Lumpur, Malaysia. IIUM Medical Journal Malaysia. 2016;15(2).
Musa R, Jamaiyah H, Azimah NM, Khairani O, Adam B. Cross-cultural Adaptation And Validation of the Malaysia Version of the Eating Disorder Examination Questionnaire (EDE-Q). Malaysian Journal of Psychiatry. 2008;17(2):55-63.
Meule A. Reconsidering the use of cut-off scores for the Eating Disorder Examination–Questionnaire. Eat Disord. 2021;29(5):480-4.
Carey M, Kupeli N, Knight R, Troop NA, Jenkinson PM, Preston C. Eating Disorder Examination Questionnaire (EDE-Q): Norms and psychometric properties in UK females and males. Psychol Assess. 2019;31(7):839-50.
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-9.
Tiong XT, Abdullah NS, Bujang MA, Ratnasingam S, Joon CK, Wee HL, et al. Validation of the Kessler's Psychological Distress Scale (K10 & K6) In A Malaysian Population. Asean Journal of Psychiatry. 2018;19(1).
Ng CG, Siddiq AA, Aida SA, Zainal NZ, Koh OH. Validation of the Malay version of the Multidimensional Scale of Perceived Social Support (MSPSS-M) among a group of medical students in Faculty of Medicine, University Malaya. Asian Journal of Psychiatry. 2010;3(1):3-6.
Vaingankar JA, Abdin E, Chong SA. Exploratory and confirmatory factor analyses of the Multidimensional Scale of Perceived Social Support in patients with schizophrenia. Compr Psychiatry. 2012;53(3):286-91.
Lee SC, Moy FM, Hairi NN. Validity and reliability of the Malay version multidimensional scale of perceived social support (MSPSS-M) among teachers. Qual Life Res. 2017;26(1):221-7.
Tavolacci MP, Ladner J, Dechelotte P. COVID-19 pandemic and eating disorders among university students. Nutrients. 2021;13(12):4294.
Shanshal AM, Hussain SA, Mahmoud MS, Saleh MA, Salih OA. Evaluating Eating Disorders among Medical Students in Baghdad, Iraq. Al-Rafidain Journal of Medical Sciences (ISSN: 2789-3219). 2022;3:6-13.
Mahar B, Warsi J, Shah T. Eating disorders and eating pattern during covid-19 pandemic: a short bulletin. Journal of Liaquat University of Medical & Health Sciences. 2021;20(02):157-62.
Taib NM, Khaiyom JH, Fauzaman J. Psychometric properties of the adapted Malay Eating Disorder Examination-Questionnaire 6.0 (EDE-Q 6.0) among university students in Malaysia. Eat Behav. 2021;42:101533.
Devoe DJ, Han A, Anderson A, Katzman DK, Patten SB, Soumbasis A, et al. The impact of the COVID‐19 pandemic on eating disorders: A systematic review. Int J Eat Disord. 2023;56(1):5-25.
Sepulveda AR, Kyriacou O, Treasure J. Development and validation of the accommodation and enabling scale for eating disorders (AESED) for caregivers in eating disorders. BMC Health Serv Res. 2009;9:171.
Tavolacci MP, Grigioni S, Richard L, Meyrignac G, Déchelotte P, Ladner J. Eating disorders and associated health risks among university students. J Nutr Educ Behav. 2015;47(5):412-20.e1.
Rø Ø, Reas DL, Rosenvinge J. The impact of age and BMI on Eating Disorder Examination Questionnaire (EDE-Q) scores in a community sample. Eating Behav. 2012;13(2):158-61.
Keane S, Clarke M, McGrath D, Farrelly N, MacHale S. Eating disorder examination questionnaire (EDE-Q): norms for female university students attending a university primary health care service in Ireland. Ir J Psychol Med. 2017;34(1):7-11.
Henderson KA, Obeid N, Buchholz A, Schubert N, Flament MF, Thai H, Goldfield GS. Coping in adolescents: A mediator between stress and disordered eating. Eating Behav. 2022;47:101626.
Mallinckrodt B, Wei M. Attachment, social competencies, social support, and psychological distress. Journal of Counseling Psychology. 2005;52(3):358.
Published
How to Cite
License
Copyright (c) 2023 Siriraj Medical Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Authors who publish with this journal agree to the following conditions:
Copyright Transfer
In submitting a manuscript, the authors acknowledge that the work will become the copyrighted property of Siriraj Medical Journal upon publication.
License
Articles are licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0). This license allows for the sharing of the work for non-commercial purposes with proper attribution to the authors and the journal. However, it does not permit modifications or the creation of derivative works.
Sharing and Access
Authors are encouraged to share their article on their personal or institutional websites and through other non-commercial platforms. Doing so can increase readership and citations.














